¿Vive con vitíligo y se pregunta si la cirugía podría ser la solución para restaurar el tono uniforme de su piel? Como un destacado... dermatólogo En Antalya, la Dra. Ebru Okyay comprende los desafíos emocionales y físicos de esta enfermedad autoinmune. El vitíligo afecta a millones de personas en todo el mundo y causa manchas blancas en la piel debido a la pérdida de melanina. Si bien los tratamientos tópicos y la fototerapia son opciones de primera línea, la cirugía ofrece esperanza para los casos estables. En esta guía completa para 2025, exploraremos quiénes cumplen los requisitos para ser considerados pacientes ideales. Candidatos a cirugía de vitíligo, los estrictos criterios de selección y qué esperar para obtener resultados óptimos.
Este artículo se basa en las últimas guías clínicas y en mi amplia experiencia en el tratamiento de pacientes con vitíligo en la clínica drebruokyay.com. Ya sea que busque despigmentación, injertos de piel o trasplante de melanocitos, comprender si es candidato es clave para lograr resultados de aspecto natural. Analicemos los aspectos esenciales para ayudarle a determinar si es un candidato adecuado.
Entendiendo el vitíligo y cuándo la cirugía se convierte en una opción
El vitíligo es una enfermedad crónica de la piel en la que el sistema inmunitario ataca a los melanocitos, las células responsables de la producción de pigmento. Esto provoca manchas despigmentadas que pueden aparecer en cualquier parte del cuerpo, comenzando a menudo en la cara, las manos o los pies. En 2025, los avances en dermatología han ampliado los horizontes terapéuticos, pero la cirugía suele reservarse para casos donde las terapias médicas resultan insuficientes.
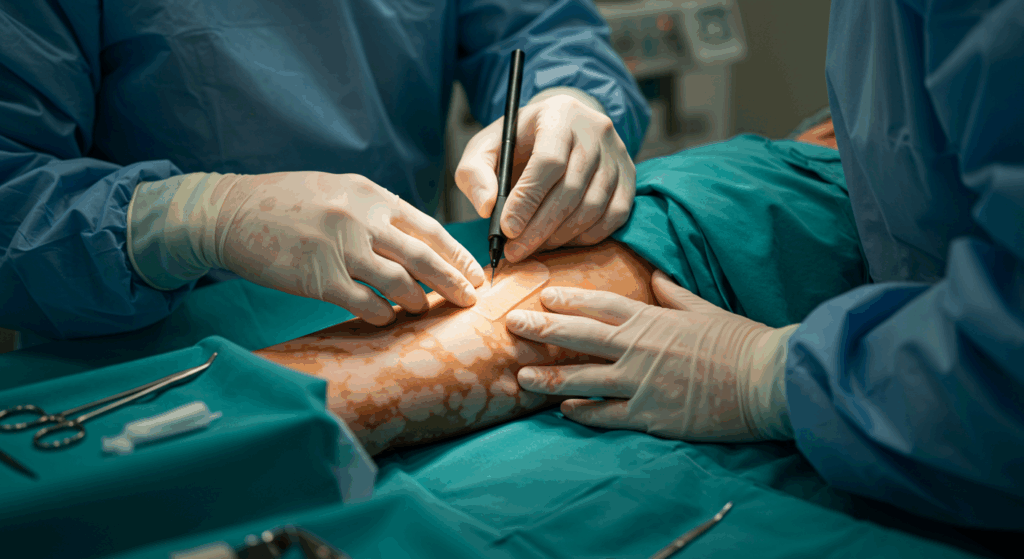
Las intervenciones quirúrgicas para el vitíligo buscan repigmentar las zonas afectadas o, en casos extensos, despigmentar la piel restante para uniformizarla. Los procedimientos comunes incluyen injertos de tejido, injertos de ampollas y técnicas de trasplante celular como la suspensión de melanocitos y queratinocitos. Sin embargo, no todos son elegibles. La cirugía es más efectiva en pacientes con vitíligo estable (es decir, sin nuevas manchas durante al menos uno o dos años) y lesiones localizadas con una superficie corporal inferior a 50%.

Tipos de vitíligo y su idoneidad quirúrgica
El vitíligo se manifiesta de diversas formas, cada una de las cuales influye en la idoneidad para la cirugía. El vitíligo segmentario, que afecta un lado o segmento del cuerpo, responde bien a la cirugía gracias a su estabilidad. El vitíligo no segmentario o generalizado, que abarca áreas más extensas, puede requerir un enfoque combinado, pero presenta mayor riesgo en procedimientos generalizados.
| Tipo de vitíligo | Descripción | Idoneidad quirúrgica |
|---|---|---|
| Vitíligo segmentario | Afecta un solo dermatoma; a menudo estable después de la progresión inicial. | Alto – Ideal para injertos localizados. |
| Vitíligo no segmentario | Manchas simétricas en ambos lados; progresivas. | Moderada: Cirugía solo para áreas focales y estables. |
| Vitíligo universal | Afecta más del 80% de la superficie corporal; despigmentación extensa. | Bajo – Se puede considerar la cirugía de despigmentación. |
| Vitíligo focal | Limitado a uno o unos pocos parches pequeños. | Alto – Excelente para trasplantes celulares. |
Para obtener más información sobre los conceptos básicos del vitíligo, consulte nuestra Conceptos básicos de la cirugía del vitíligo guía.
En mi práctica, he visto cómo la cirugía ha transformado la vida de pacientes con manchas resistentes en zonas visibles como los labios o los párpados, donde camuflarse es difícil. Sin embargo, el éxito depende de una selección precisa de los pacientes para minimizar las recurrencias y las complicaciones.
Criterios clave de selección para candidatos a cirugía de vitíligo
Seleccionar lo correcto Candidatos a cirugía de vitíligo Es tanto un arte como una ciencia. Según las Directrices Internacionales para el Vitíligo de 2025, los criterios se centran en la estabilidad de la enfermedad, las características de la lesión, la salud del paciente y la preparación psicológica. Analicemos los factores esenciales que determinan la elegibilidad.
1. Estabilidad y duración de la enfermedad
La clave para ser candidato es la estabilidad. El vitíligo activo, con placas que se extienden, contraindica la cirugía, ya que los injertos pueden fallar o desencadenar el fenómeno de Koebner (nuevas lesiones en las zonas de traumatismo). Los candidatos ideales tienen:
- No se deben presentar lesiones nuevas o en expansión durante al menos 12 a 24 meses.
- Duración de la enfermedad de más de 2 años, lo que indica fase de agotamiento.
- Respuesta a terapias médicas previas como la UVB de banda estrecha, confirmando la estabilidad.
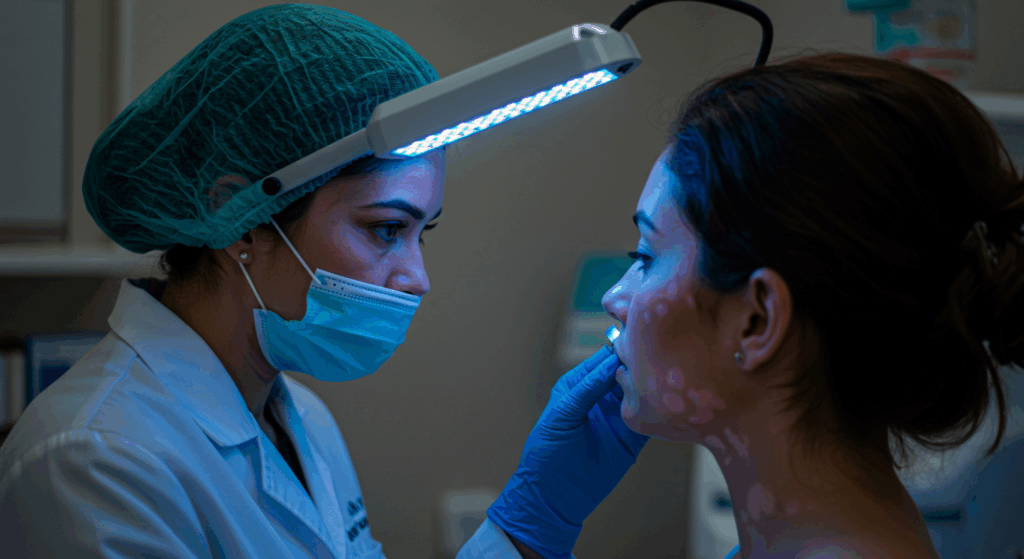
En mi clínica de Antalya, utilizamos exámenes con lámpara de Wood y fotografías seriadas para verificar la estabilidad durante 6 a 12 meses antes de continuar.
2. Tamaño, ubicación y características de la lesión
No todas las manchas de vitíligo son quirúrgicas. Las lesiones pequeñas y bien definidas (menores de 5 cm²) en zonas cosméticamente sensibles, como el rostro o las manos, son las principales dianas. Las manchas acrómicas, foliculares o hipopigmentadas se repigmentan mejor que las zonas labiales o acrales (manos/pies), que tienen un riego sanguíneo más deficiente.
| Ubicación de la lesión | Tasa de éxito quirúrgico | Procedimiento recomendado |
|---|---|---|
| Cara/Cuello | 80-90% | Suspensión de melanocitos o injerto de ampollas. |
| Tronco/Extremidades | 70-85% | Injerto de tejido para áreas más grandes. |
| Manos/Pies | 50-70% | Limitado a parches pequeños y estables; se prefieren los métodos celulares. |
| Labios/Párpados | 60-80% | Técnicas especializadas de microinjerto. |
Evite la cirugía en parches inestables, confluentes o muy grandes (>20 cm), ya que las tasas de repigmentación caen por debajo de 50%.
3. Edad del paciente, tipo de piel y estado de salud
La edad influye: los adultos mayores de 18 años con piel madura cicatrizan mejor, aunque los adolescentes con vitíligo estable pueden requerir supervisión. Los tipos de piel Fitzpatrick I-III (piel más clara) muestran mayor éxito, pero los tipos IV-VI pueden beneficiarse de terapias complementarias.
Los criterios de salud excluyen a los candidatos con:
- Enfermedades autoinmunes activas (por ejemplo, tiroiditis, a menos que esté controlada).
- Tendencia conocida a la formación de cicatrices queloides.
- Diabetes no controlada, hipertensión o antecedentes de tabaquismo (aumenta el riesgo de fracaso en 30%).
- Embarazo o lactancia (aplazar 6 meses).
El análisis de sangre preoperatorio, incluida la función tiroidea y los niveles de vitamina D, es obligatorio para descartar comorbilidades.
4. Factores psicológicos y de estilo de vida
La cirugía no es solo física; la preparación emocional es crucial. Los candidatos deben tener expectativas realistas: la repigmentación es de 70-90% en el mejor de los casos, y la recurrencia es posible en 20%. Las personas con tendencias dismórficas corporales o ansiedad alta podrían necesitar terapia previa.
En cuanto al estilo de vida, es fundamental comprometerse con los cuidados posoperatorios (protección solar, evitar traumatismos). En 2025, priorizamos la toma de decisiones compartida, analizando alternativas como los inhibidores de JAK si la cirugía no es la solución ideal.
Explore las técnicas quirúrgicas en detalle a través de nuestro Técnicas y métodos en la cirugía del vitíligo artículo.
Evaluación preoperatoria: evaluación de su candidatura
Una evaluación exhaustiva es la clave para una cirugía de vitíligo exitosa. En drebruokyay.com en Antalya, nuestro proceso comienza con una consulta detallada para evaluar todos los criterios de selección.
Protocolo preoperatorio paso a paso
1. Revisión del historial médico: Documente la aparición y progresión del vitíligo, los antecedentes familiares y los tratamientos previos. Evalúe contraindicaciones como la inmunosupresión.
2. Examen físico: Utilice la dermatoscopia y la luz ultravioleta para mapear las lesiones, evaluar la viabilidad del sitio donante (por ejemplo, el muslo para injertos) y evaluar la laxitud de la piel.
3. Documentación fotográfica: Las imágenes de referencia rastrean la estabilidad a lo largo de los seguimientos.
4. Pruebas de laboratorio: El hemograma completo, el panel tiroideo, la HbA1c y los marcadores autoinmunes garantizan la seguridad.
5. Evaluación psicológica: Las evaluaciones breves miden la motivación y los mecanismos de afrontamiento.
Herramientas de diagnóstico avanzadas en 2025
Las herramientas modernas mejoran la precisión: la microscopía confocal visualiza la actividad de los melanocitos, mientras que el mapeo de lesiones asistido por IA predice el potencial de repigmentación. Esto ayuda a adaptar los procedimientos, lo que aumenta el éxito de los candidatos cualificados para el 85%.
| Paso de evaluación | Propósito | Duración prevista |
|---|---|---|
| Historia y examen | Identificar riesgos y estabilidad | 30-45 minutos |
| Pruebas de laboratorio | Descartar comorbilidades | 1-2 semanas para obtener resultados |
| Imágenes/dermoscopia | Caracterización de la lesión | 20 minutos |
| Asesoramiento | Establecer expectativas | 45 minutos |
Si las evaluaciones confirman la candidatura, procedemos a la planificación. Para obtener indicaciones, consulte nuestra Guía de indicaciones para la cirugía del vitíligo.
Riesgos, resultados y gestión a largo plazo para los candidatos
Incluso ideal Candidatos a cirugía de vitíligo Afrontan riesgos, pero las decisiones informadas los mitigan. Los resultados varían, con una repigmentación de 70-95% en lesiones faciales, según 2025 estudios.
Riesgos potenciales y cómo minimizarlos
Los riesgos comunes incluyen infección (5%), cicatrización (10-15%) o fallo parcial del injerto (20%). En pieles más oscuras, se producen desajustes de hipopigmentación. Minimizamos estos riesgos mediante técnicas estériles, antibióticos y láminas de silicona para cicatrices.
- Cuidados perioperatorios: Higiene estricta y cura de heridas.
- Terapias complementarias: La fototerapia postoperatoria mejora la toma del injerto.
- Hacer un seguimiento: Cheques mensuales por 6 meses.
Resultados esperados y tasas de éxito
El éxito se define como una repigmentación >75% al año. Factores que aumentan las tasas: Enfermedad estable, zonas faciales y terapias combinadas. En mi experiencia, el 85% de los candidatos logra resultados satisfactorios, con una mejora en la igualación del color a lo largo de 18 meses.
| Procedimiento | Tasa de éxito (repigmentación %) | Perfil del candidato ideal |
|---|---|---|
| Injerto de piel | 70-85% | Pequeñas manchas estables en el tronco. |
| Injerto de ampolla | 80-90% | Lesiones faciales; morbilidad mínima del donante. |
| Trasplante de melanocitos | 75-95% | Áreas extensas; buenos melanocitos donantes. |
| Despigmentación | Uniformidad 90-100% | Vitíligo extenso (>50% BSA). |
A largo plazo, 10-20% presenta recurrencia, que se controla con UVB de mantenimiento. Consulte los resultados en nuestro... Resultados y tasas de éxito de la cirugía del vitíligo correo.
Conclusión
Conclusiones clave
- Ideal Candidatos a cirugía de vitíligo tener una enfermedad estable durante 1-2 años, lesiones localizadas y ninguna contraindicación de salud importante.
- Las evaluaciones preoperatorias que incluyen exámenes, análisis de laboratorio y asesoramiento garantizan la seguridad y expectativas realistas.
- Los resultados quirúrgicos alcanzan la repigmentación 70-95%, con riesgos minimizados mediante atención experta.
- En 2025, clínicas de Antalya como drebruokyay.com ofrecerán cirugía de vitíligo avanzada y personalizada para obtener resultados transformadores.
Próximos pasos
¿Estás considerando la cirugía de vitíligo? Empieza por:
- Seguimiento de sus lesiones para garantizar su estabilidad durante 6 meses.
- Consultar con un dermatólogo para una evaluación integral.
- Programe una consulta gratuita en drebruokyay.com para discutir su candidatura.
- Explore opciones no quirúrgicas si la cirugía aún no es adecuada.
La Dra. Ebru Okyay se dedica a empoderar a los pacientes con vitíligo con atención basada en evidencia en Antalya.
Preguntas frecuentes (FAQ)
¿Quién es el candidato ideal para la cirugía de vitíligo?
Los candidatos ideales tienen vitíligo estable durante al menos 12 meses, manchas localizadas, buena salud y expectativas realistas. Las lesiones faciales suelen ofrecer los mejores resultados.
¿Cuánto tiempo debe permanecer estable el vitíligo antes de la cirugía?
Normalmente, se requieren de 1 a 2 años sin necesidad de nuevos parches. Esto reduce riesgos como el fenómeno de Koebner y mejora la supervivencia del injerto.
¿Qué condiciones de salud descalifican a alguien para la cirugía de vitíligo?
Infecciones activas, enfermedades autoinmunes no controladas, trastornos de la coagulación o antecedentes de cicatrices queloides. Se requiere dejar de fumar de 4 a 6 semanas antes.
¿Es dolorosa la cirugía de vitíligo?
La anestesia local minimiza las molestias durante el procedimiento. El dolor posoperatorio se controla con analgésicos suaves durante 3 a 5 días.
¿Cuál es el tiempo de recuperación después de la cirugía de vitíligo?
El tiempo de recuperación para la cicatrización de la herida es de 7 a 14 días. La repigmentación completa tarda de 3 a 6 meses, con restricciones en la exposición al sol y otras actividades.
¿Puede la cirugía curar el vitíligo por completo?
La cirugía repigmenta áreas específicas, pero no cura el proceso autoinmune subyacente. La recurrencia es posible en el 10-20% de los casos.
¿La cirugía de vitíligo es adecuada para niños?
Rara vez; sólo para adolescentes mayores de 16 años con vitíligo focal estable después de una terapia médica fallida y el consentimiento de los padres.
¿Cuánto cuesta la cirugía de vitíligo en Antalya?
El costo varía entre $2,000 y $5,000, dependiendo del procedimiento y el tamaño de la lesión. Las consultas son gratuitas en drebruokyay.com.
