El eccema, también conocido como dermatitis atópica, es una afección cutánea inflamatoria crónica que afecta a millones de personas en todo el mundo. Caracterizado por picazón, enrojecimiento, sequedad y agrietamiento de la piel, el eccema puede afectar significativamente la calidad de vida de una persona, afectando el sueño, el trabajo y las interacciones sociales. Encontrar tratamientos eficaces es crucial para controlar los síntomas y mejorar la vida de quienes viven con esta afección. Entre las diversas opciones terapéuticas disponibles, Corticosteroides tópicos Destacan como una piedra angular en el manejo de los brotes de eccema. Esta guía completa profundizará en el mundo de Corticosteroides tópicos, explorando sus mecanismos de acción, diferentes tipos, uso adecuado, posibles efectos secundarios y su papel en el panorama más amplio de los tratamientos del eczema.

Entendiendo la carga del eczema
Vivir con eccema es más que simplemente lidiar con una erupción. La picazón persistente y a menudo intensa puede ser debilitante, provocando noches de insomnio y fatiga diurna. Los síntomas visibles en la piel, como enrojecimiento, descamación y supuración, pueden causar un gran malestar emocional, afectando la autoestima y la confianza social. Los niños con eccema pueden sufrir acoso escolar o sentirse cohibidos por su apariencia, mientras que los adultos pueden ver su condición impactando su rendimiento laboral y sus relaciones sociales.
La naturaleza impredecible del eccema, con sus ciclos de brotes y remisiones, añade otra capa de complejidad al manejo de la afección. Las personas a menudo se encuentran en constante alerta, intentando identificar y evitar posibles desencadenantes como alérgenos, irritantes, estrés e incluso cambios climáticos. Esta vigilancia constante puede ser mentalmente agotadora y afectar significativamente el bienestar general.
Además, la incomodidad y la aparición del eccema pueden provocar complicaciones secundarias, como infecciones cutáneas causadas por el rascado. La inflamación crónica asociada al eccema también puede tener consecuencias más amplias para la salud, aumentando potencialmente el riesgo de otras afecciones como el asma y la fiebre del heno, en lo que a menudo se conoce como la marcha atópica.
La búsqueda de tratamientos eficaces para el eccema puede ser un proceso largo y frustrante para muchos. Los remedios de venta libre pueden proporcionar un alivio temporal para los síntomas leves, pero a menudo se necesitan medicamentos con receta para controlar el eccema de moderado a grave. Entre estos tratamientos con receta, Corticosteroides tópicos Han sido un pilar durante décadas y ofrecen un alivio significativo de la inflamación y la picazón.

La agonía de la picazón y la inflamación
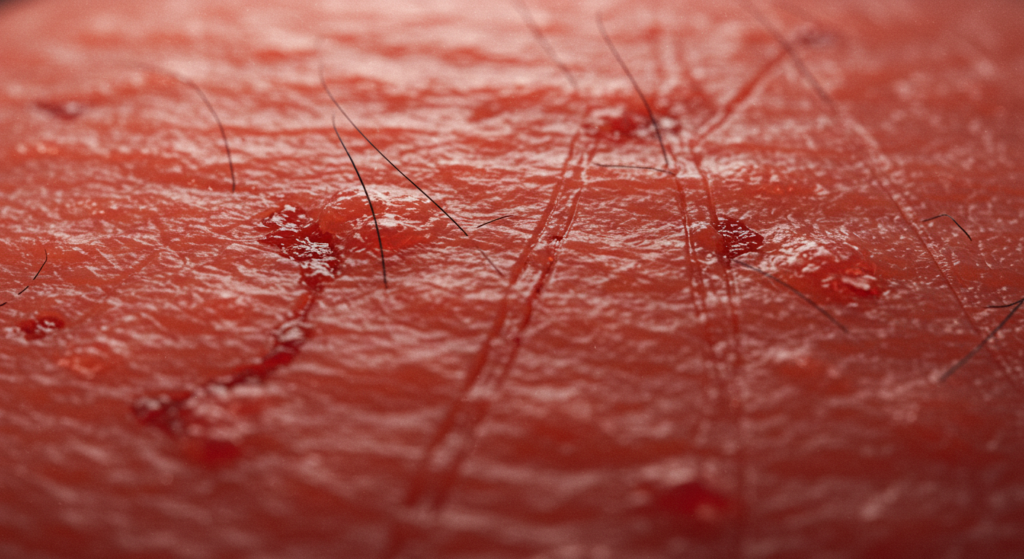
Imagine una picazón persistente e incesante que no se puede calmar rascándose. Esta es la realidad diaria de muchas personas que viven con eczema. La picazón puede ser tan intensa que interrumpe el sueño, dificultando la concentración durante el día. Rascarse, aunque proporciona un alivio temporal, a menudo agrava la inflamación, creando un círculo vicioso de picazón y rascado que puede ser increíblemente difícil de romper.
La inflamación asociada al eccema no es solo superficial. Implica una compleja interacción entre células inmunitarias y mediadores inflamatorios que causan el enrojecimiento, la hinchazón y la sensación de calor característicos en las zonas afectadas. Esta inflamación altera la función de barrera natural de la piel, haciéndola más susceptible a la sequedad, la irritación y las infecciones.
La aparición del eccema también puede ser una fuente de gran angustia. Las manchas rojas y escamosas pueden aparecer en cualquier parte del cuerpo, pero son comunes en las manos, los pies, los tobillos, las muñecas, el cuello, la parte superior del pecho, los párpados y alrededor de la boca. En los bebés, el eccema suele afectar la cara, el cuero cabelludo, la superficie externa de los brazos y las piernas, el pecho y la espalda. La visibilidad de estos síntomas puede provocar sentimientos de vergüenza, pudor y aislamiento social.
El impacto del eccema va más allá de los síntomas físicos. Estudios han demostrado que las personas con eccema son más propensas a experimentar ansiedad, depresión y otros trastornos de salud mental. La naturaleza crónica de la afección, los brotes impredecibles y la necesidad constante de autocuidado pueden afectar significativamente el bienestar mental y emocional.
Por lo tanto, encontrar un tratamiento que controle eficazmente la picazón y la inflamación es fundamental para mejorar la calidad de vida de las personas con eccema. Si bien no existe cura para el eccema, existen diversos tratamientos para controlar los síntomas y prevenir los brotes. Corticosteroides tópicos desempeñan un papel crucial en este tratamiento, ofreciendo una forma potente de reducir la inflamación y aliviar la picazón debilitante.
Corticosteroides tópicos: una solución eficaz para el eccema
Corticosteroides tópicosLos esteroides tópicos, a menudo conocidos como esteroides tópicos, son medicamentos recetados que se aplican directamente sobre la piel para reducir la inflamación y la picazón asociadas con el eccema. Son versiones sintéticas del cortisol, una hormona producida naturalmente por las glándulas suprarrenales y con propiedades antiinflamatorias.
Cómo funcionan los corticosteroides tópicos
Cuando se aplica sobre la piel, Corticosteroides tópicos Actúan suprimiendo la respuesta del sistema inmunitario en la zona tratada. En el caso del eccema, el sistema inmunitario reacciona de forma exagerada a ciertos desencadenantes, lo que provoca inflamación. Corticosteroides tópicos ayudar a calmar esta respuesta inmune hiperactiva mediante:
- Reducir la producción de sustancias químicas inflamatorias: Inhiben la liberación de sustancias como las citocinas y las prostaglandinas que contribuyen a la inflamación, el enrojecimiento y la hinchazón.
- Constricción de los vasos sanguíneos: Esto ayuda a reducir el enrojecimiento y la hinchazón de la piel afectada.
- Suprimir la actividad de las células inmunes: Pueden reducir el número y la actividad de las células inmunes involucradas en el proceso inflamatorio de la piel.
Al apuntar a estos mecanismos clave, Corticosteroides tópicos Alivia eficazmente los síntomas primarios del eczema, como picazón, enrojecimiento e hinchazón, permitiendo que la piel sane.
Diferentes potencias de corticosteroides tópicos
Corticosteroides tópicos Están disponibles en diversas concentraciones o potencias, desde leves hasta muy potentes. La potencia de un corticosteroide tópico se refiere a su capacidad para reducir la inflamación. La elección de la potencia depende de varios factores, entre ellos:
- Gravedad del eczema: Los brotes más graves a menudo requieren corticosteroides de mayor potencia para un control efectivo.
- Ubicación del eczema: Las zonas de piel más fina, como la cara y las ingles, son más susceptibles a los efectos secundarios y suelen requerir corticosteroides de menor potencia. Las zonas de piel más gruesa, como las palmas de las manos y las plantas de los pies, pueden requerir corticosteroides de mayor potencia para una penetración adecuada.
- Edad del paciente: Los bebés y los niños pequeños generalmente requieren corticosteroides de menor potencia debido a su piel más delgada y al mayor riesgo de absorción sistémica.
- Respuesta del paciente al tratamiento: Si un corticosteroide de menor potencia no es efectivo, un médico puede recetar uno de mayor potencia.
A continuación se presenta una clasificación general de Corticosteroides tópicos por potencia, junto con algunos ejemplos (tenga en cuenta que las marcas específicas y la disponibilidad pueden variar):
Muy alta potencia: Estos son los más fuertes Corticosteroides tópicos Se suelen usar para el eccema severo en zonas de piel gruesa. Algunos ejemplos son:
- Dipropionato de betametasona 0,05% (aumentado)
- Propionato de clobetasol 0,05%
Alta potencia: Se utilizan para el eccema de moderado a severo en diversas partes del cuerpo, excepto la cara y las ingles durante períodos prolongados. Algunos ejemplos incluyen:
- Dipropionato de betametasona 0,05%
- Fluocinonida 0.05%
- Furoato de mometasona 0,1%
Potencia media: Se suelen usar para el eccema leve o moderado y pueden usarse en zonas más sensibles bajo estricta supervisión médica. Algunos ejemplos incluyen:
- Valerato de betametasona 0,1%
- Acetónido de triamcinolona 0.1%
Baja potencia: Estos son los más suaves Corticosteroides tópicos Se utilizan a menudo para eccemas leves, terapia de mantenimiento y en zonas sensibles como la cara y las ingles. También se utilizan comúnmente en bebés y niños pequeños. Algunos ejemplos incluyen:
- Hidrocortisona 1% y 2.5%
- Desonida 0.05%
Es fundamental utilizar la Corticosteroide tópico Con la potencia prescrita por su profesional de la salud y siguiendo atentamente sus instrucciones. Usar un corticosteroide de mayor potencia de la necesaria o por más tiempo del recomendado puede aumentar el riesgo de efectos secundarios.
Aplicación adecuada de corticosteroides tópicos
Aplicando Corticosteroides tópicos Administrarlos correctamente es esencial para maximizar su eficacia y minimizar el riesgo de efectos secundarios. A continuación, se presentan algunas pautas generales:
- Lávese y séquese las manos: Esto ayuda a prevenir la infección.
- Aplicar una capa fina: Use solo la cantidad de medicamento necesaria para cubrir la piel afectada. Aplicar una capa gruesa no mejora la eficacia del medicamento y puede aumentar el riesgo de efectos secundarios. Una regla general es usar la "unidad de la yema del dedo" (UTD), que es la cantidad de crema o ungüento exprimida desde la punta del dedo índice de un adulto hasta el primer pliegue. Una UTD suele ser suficiente para cubrir un área del tamaño aproximado de ambos lados de la mano de un adulto.
- Frótalo suavemente: Frote el medicamento suavemente hasta que desaparezca en la piel.
- Lávese las manos nuevamente: A menos que esté tratando sus manos, lávelas inmediatamente después de aplicar el medicamento para evitar que se propague a otras áreas.
- Úselo según las indicaciones: Aplicar el Corticosteroide tópico Con la frecuencia y la duración prescritas por su profesional de la salud. No lo use con más frecuencia ni por más tiempo del recomendado.
- Evite los vendajes oclusivos a menos que se le indique lo contrario: Los apósitos oclusivos, como vendajes o envolturas plásticas, pueden aumentar la absorción del medicamento y pueden recomendarse en algunos casos, pero solo deben usarse bajo la guía de un profesional de la salud.
- Hidratar regularmente: Los emolientes (humectantes) son cruciales para el manejo del eccema. Ayudan a hidratar la piel y a restaurar la barrera cutánea. Aplique abundante crema hidratante a lo largo del día, especialmente después del baño y cuando sienta la piel seca. Generalmente, se recomienda aplicar la crema hidratante después de... Corticosteroide tópico ha sido absorbido.
Su profesional de la salud podría darle instrucciones específicas según sus necesidades individuales y la ubicación y gravedad de su eccema. Es importante seguir estas instrucciones cuidadosamente.
Posibles efectos secundarios de los corticosteroides tópicos
En Corticosteroides tópicos Aunque generalmente son seguros y eficaces cuando se usan según lo prescrito, pueden tener efectos secundarios, especialmente con el uso prolongado de formulaciones de alta potencia o una aplicación incorrecta. Estos efectos secundarios pueden clasificarse en general en locales (que afectan la piel en el lugar de aplicación) y sistémicos (que afectan al organismo en su conjunto).
Efectos secundarios locales:
- Adelgazamiento de la piel (atrofia): Esta es una de las preocupaciones más comunes con el uso prolongado de potentes Corticosteroides tópicosLa piel puede volverse más fina, más frágil y más propensa a hematomas o desgarros.
- Telangiectasia: Se trata de vasos sanguíneos pequeños y dilatados que pueden hacerse visibles en la superficie de la piel y a menudo aparecen como finas líneas rojas.
- Estrías: Estas pueden aparecer en áreas donde la piel se ha estirado, como la ingle, las axilas o los senos.
- Acné o foliculitis: Corticosteroides tópicos A veces puede desencadenar o empeorar el acné o causar inflamación de los folículos pilosos (foliculitis) en el área tratada.
- Dermatitis perioral: Se trata de una erupción que puede desarrollarse alrededor de la boca, a menudo asociada con el uso de potentes Corticosteroides tópicos en la cara.
- Cambios en el color de la piel (hipopigmentación o hiperpigmentación): La piel tratada puede volverse más clara o más oscura que la piel circundante.
- Dermatitis de contacto: En algunos casos, las personas pueden desarrollar una reacción alérgica al Corticosteroide tópico en sí mismo o a los ingredientes del vehículo (crema, ungüento, etc.).
- Mayor riesgo de infecciones de la piel: Uso prolongado de Corticosteroides tópicos A veces puede suprimir la respuesta inmunitaria local, aumentando potencialmente el riesgo de infecciones cutáneas bacterianas, fúngicas o virales.
Efectos secundarios sistémicos:
Efectos secundarios sistémicos de Corticosteroides tópicos Son poco frecuentes cuando se usan correctamente y por períodos limitados. Sin embargo, son más probables con el uso prolongado de corticosteroides de alta potencia en áreas extensas del cuerpo, especialmente bajo oclusión. Los posibles efectos secundarios sistémicos incluyen:
- Supresión suprarrenal: Esto ocurre cuando la producción natural de cortisol del cuerpo se suprime debido a la absorción del esteroide tópico en el torrente sanguíneo. Esto suele ser reversible al suspender el medicamento, pero puede ser grave si no se trata adecuadamente.
- Retraso del crecimiento en niños: En casos raros, el uso prolongado de potentes Corticosteroides tópicos En los niños puede afectar su crecimiento.
- Aumento de los niveles de azúcar en sangre: Corticosteroides tópicos A veces puede provocar un aumento temporal de los niveles de azúcar en sangre, especialmente en personas con diabetes.
- Cataratas o glaucoma: Estas afecciones oculares rara vez se han asociado con el uso de Corticosteroides tópicos, especialmente con el uso prolongado alrededor de los ojos.
Es importante hablar sobre los posibles efectos secundarios con su profesional de la salud e informar cualquier síntoma inusual o cambio en la piel que se presente durante el tratamiento. Ellos pueden ayudarle a evaluar los beneficios y los riesgos. Corticosteroides tópicos y vigilarle para detectar cualquier efecto secundario.
Minimizar el riesgo de efectos secundarios
Varias estrategias pueden ayudar a minimizar el riesgo de efectos secundarios. Corticosteroides tópicos:
- Utilice la potencia efectiva más baja: Su proveedor de atención médica le recetará el corticosteroide de menor potencia que probablemente controle su eczema.
- Úselo durante el menor tiempo posible: Corticosteroides tópicos Generalmente, debe usarse por períodos cortos para controlar los brotes. Para el tratamiento de mantenimiento, su médico podría recomendar el uso intermitente o un corticosteroide de menor potencia.
- Aplicar sólo en las zonas afectadas: Evite aplicar el medicamento sobre piel no afectada.
- Utilice la cantidad correcta: Siga la regla de la unidad de la yema del dedo o las instrucciones de su médico para evitar la aplicación excesiva.
- Evite el uso prolongado de corticosteroides de alta potencia en zonas sensibles: La cara, la ingle y las axilas son más propensas a sufrir efectos secundarios y, por lo general, deben tratarse con corticosteroides de menor potencia u otros medicamentos.
- Considere la terapia intermitente: Para el eccema crónico, su médico puede recomendar el uso de Corticosteroides tópicos durante unos días o semanas para controlar un brote, seguido de un descanso o el uso de otros tratamientos como emolientes o inhibidores tópicos de la calcineurina.
- Seguimiento regular con su proveedor de atención médica: Los chequeos regulares le permiten a su médico monitorear su condición y ajustar su plan de tratamiento según sea necesario.
Combinación de corticosteroides tópicos con otros tratamientos para el eccema
Corticosteroides tópicos Se suelen usar junto con otros tratamientos para el eccema para brindar un manejo integral de la afección. Estos incluyen:
- Emolientes (humectantes): Estos son la piedra angular del tratamiento del eccema. El uso regular y abundante de emolientes ayuda a hidratar la piel, restaurar la barrera cutánea y reducir la sequedad y el picor. Deben aplicarse con frecuencia a lo largo del día, especialmente después del baño.
- Inhibidores tópicos de la calcineurina (ITC): Se trata de cremas y ungüentos no esteroides de venta con receta que también ayudan a reducir la inflamación de la piel. Se suelen utilizar como alternativa a... Corticosteroides tópicos, especialmente para tratamientos a largo plazo o en zonas sensibles como el rostro y el cuello. Algunos ejemplos son el tacrolimús y el pimecrolimús.
- Crisaborola: Este es otro medicamento tópico no esteroideo que actúa inhibiendo una enzima llamada fosfodiesterasa 4 (PDE4), que desempeña un papel en la inflamación.
- Medicamentos sistémicos: Para el eccema grave que no responde adecuadamente a los tratamientos tópicos, se pueden recetar medicamentos orales como corticosteroides, inmunosupresores (p. ej., ciclosporina, metotrexato, azatioprina) o fármacos biológicos (p. ej., dupilumab, tralokinumab, upadacitinib, abrocitinib). Estos medicamentos actúan en todo el organismo para suprimir el sistema inmunitario y reducir la inflamación.
- Fototerapia (terapia de luz): Esto implica exponer la piel a tipos específicos de luz ultravioleta (UV) bajo supervisión médica. Puede ayudar a reducir la inflamación y la picazón en algunas personas con eccema.
- Evitar desencadenantes: Identificar y evitar los desencadenantes conocidos del eczema, como ciertos alérgenos o irritantes, puede ayudar a prevenir los brotes.
- Manejo del estrés: El estrés a veces puede empeorar los síntomas del eccema. Practicar técnicas para reducir el estrés, como el yoga, la meditación o ejercicios de respiración profunda, puede ser beneficioso.
Su proveedor de atención médica desarrollará un plan de tratamiento personalizado según la gravedad de su eczema, su edad, su salud general y su respuesta a diferentes tratamientos. Corticosteroides tópicos A menudo desempeñan un papel clave en este plan, en particular en el manejo de los brotes agudos.
Corticosteroides tópicos para diferentes grupos de edad
El uso de Corticosteroides tópicos En bebés, niños y adultos se requiere una consideración cuidadosa debido a las diferencias en el grosor de la piel, la relación entre la superficie y el peso corporal y el potencial de absorción sistémica.
Bebés y niños pequeños:
Los bebés y los niños pequeños tienen una piel más fina y una mayor relación superficie-peso corporal en comparación con los adultos, lo que significa que son más susceptibles a la absorción sistémica de Corticosteroides tópicosPor lo tanto, generalmente se prefieren los corticosteroides de menor potencia para este grupo de edad, y deben usarse con moderación y bajo estrecha supervisión médica. Los corticosteroides de alta potencia suelen evitarse en bebés y niños pequeños, a menos que un médico los recomiende específicamente. dermatólogo.
Niños mayores y adolescentes:
Los niños mayores y los adolescentes a menudo pueden utilizar una gama más amplia de Corticosteroide tópico Las potencias varían según la gravedad y la ubicación del eccema. Sin embargo, sigue siendo importante usar la potencia efectiva más baja y evitar el uso prolongado de corticosteroides de alta potencia, especialmente en la cara y las ingles.
Adultos:
Los adultos con eczema pueden requerir una variedad de Corticosteroide tópico Las potencias varían según la gravedad y la localización de los síntomas. Generalmente, toleran corticosteroides de mayor potencia durante periodos cortos para controlar los brotes graves. Sin embargo, se aplican los mismos principios de usar la potencia efectiva más baja y evitar el uso prolongado de corticosteroides de alta potencia, especialmente en zonas sensibles.
En todos los grupos de edad, es fundamental seguir cuidadosamente las instrucciones del proveedor de atención médica con respecto al tipo, la potencia, la frecuencia y la duración del tratamiento. Corticosteroide tópico usar.
Abordando inquietudes y conceptos erróneos comunes sobre los corticosteroides tópicos
Corticosteroides tópicos A veces se perciben con aprensión debido a la preocupación por sus posibles efectos secundarios, a menudo derivados de desinformación o confusión con los corticosteroides orales o inyectables, que pueden tener efectos secundarios sistémicos más significativos. Es importante abordar algunas inquietudes y conceptos erróneos comunes:
- “Los esteroides tópicos adelgazarán mi piel de forma permanente”. Si bien el uso prolongado de potentes antiinflamatorios puede causar adelgazamiento de la piel, Corticosteroides tópicosGeneralmente es reversible al suspender el medicamento. Usar la dosis adecuada y seguir las instrucciones del médico puede ayudar a minimizar este riesgo.
- “Los esteroides tópicos son adictivos”. Corticosteroides tópicos No son adictivos en el sentido tradicional. Sin embargo, cuando los síntomas del eccema mejoran con su uso, las personas pueden recurrir a ellos durante los brotes. Es importante colaborar con su profesional de la salud para desarrollar un plan de tratamiento integral que incluya emolientes y otras estrategias para prevenir brotes frecuentes.
- “Debería evitar todos los esteroides”. Es importante distinguir entre los corticosteroides tópicos, que se aplican sobre la piel, y los corticosteroides sistémicos (orales o inyectables), que tienen un efecto más amplio en el organismo y pueden tener efectos secundarios más importantes. Corticosteroides tópicos Son una herramienta valiosa para controlar el eczema cuando se utilizan correctamente.
- “Los remedios naturales siempre son mejores que los esteroides tópicos”. Si bien algunos remedios naturales pueden brindar alivio para el eczema leve, a menudo no son suficientes para controlar la inflamación moderada a severa. Corticosteroides tópicos Suelen ser necesarios para controlar eficazmente los brotes y prevenir daños cutáneos a largo plazo. Es recomendable consultar con su profesional de la salud sobre todas las opciones de tratamiento, incluidas las terapias complementarias y alternativas.
Es fundamental tener una conversación abierta y honesta con su proveedor de atención médica acerca de sus inquietudes con respecto a Corticosteroides tópicosPueden brindarle información precisa, responder a sus preguntas y ayudarlo a tomar decisiones informadas sobre su tratamiento.
El futuro de los corticosteroides tópicos y el tratamiento del eccema
En Corticosteroides tópicos han sido un pilar en el tratamiento del eccema durante décadas, la investigación continúa mejorando nuestra comprensión del eccema y desarrollando terapias nuevas y mejoradas. La investigación en curso en el campo de Corticosteroides tópicos Se centra en:
- Desarrollo de formulaciones más seguras y específicas: Los científicos están trabajando en nuevas formas de administrar corticosteroides a la piel que minimicen la absorción sistémica y reduzcan el riesgo de efectos secundarios locales.
- Combinación de corticosteroides con otros ingredientes activos: Algunos productos combinados contienen un corticosteroide junto con otro medicamento, como un antibiótico o un antimicótico, para abordar necesidades específicas.
- Explorando el papel del microbioma de la piel: La investigación sobre las bacterias, hongos y virus que viven en nuestra piel está conduciendo a nuevos conocimientos sobre el eczema y posibles tratamientos dirigidos al microbioma de la piel.
Además de los avances en Corticosteroides tópicosSe han producido avances significativos en el desarrollo de nuevos tratamientos no esteroideos para el eccema, como los inhibidores tópicos de JAK y los fármacos biológicos que actúan sobre vías inflamatorias específicas. Estas nuevas terapias ofrecen opciones adicionales para las personas con eccema, especialmente para quienes no responden bien al tratamiento o no lo toleran. Corticosteroides tópicos.
Es probable que el futuro del tratamiento del eczema implique un enfoque personalizado, en el que los proveedores de atención médica adapten los planes de tratamiento en función del tipo y la gravedad específicos del eczema de cada individuo, sus desencadenantes, su respuesta a diferentes terapias y su salud general. Corticosteroides tópicos Probablemente seguirá desempeñando un papel importante en este enfoque personalizado, en particular para el control rápido de los brotes.
Conclusión: Encontrar alivio con corticosteroides tópicos
Vivir con eczema puede ser un desafío, pero existen tratamientos efectivos para ayudar a controlar los síntomas y mejorar la calidad de vida. Corticosteroides tópicos Han sido una piedra angular de la terapia del eczema durante muchos años, proporcionando un alivio significativo de la inflamación y la picazón cuando se usan correctamente.
Entendiendo las diferentes potencias de Corticosteroides tópicos, cómo aplicarlos correctamente y sus posibles efectos secundarios son cruciales para un uso seguro y eficaz. Es fundamental colaborar estrechamente con su profesional de la salud para desarrollar un plan de tratamiento personalizado que incluya Corticosteroides tópicos cuando sea apropiado, junto con emolientes y otras estrategias para controlar su eczema.
Si bien las preocupaciones sobre los efectos secundarios son comprensibles, cuando se utiliza bajo supervisión médica y durante la duración recomendada, Corticosteroides tópicos Generalmente son seguros y pueden brindar el alivio necesario de los síntomas debilitantes del eccema. Al mantenerse informado, comunicarse abiertamente con su profesional de la salud y adherirse a su plan de tratamiento, puede controlar eficazmente su eccema y vivir una vida más cómoda y plena. Recuerde que no está solo en este proceso y que existen muchos recursos y sistemas de apoyo disponibles para ayudarle a afrontar los desafíos de vivir con eccema.
Descubra la experiencia de la Dra. Ebru Okyay, su médico de confianza. dermatólogo en AntalyaYa sea que esté buscando abordar problemas médicos de la piel o mejorar su belleza natural con tratamientos cosméticos, el Dr. Okyay está aquí para ayudarlo. Con atención personalizada y técnicas avanzadas, lograr sus objetivos para la piel nunca ha sido tan fácil.