El angioedema es una afección grave que se caracteriza por la inflamación bajo la superficie de la piel. A menudo, aunque no siempre, se presenta junto con urticaria, una reacción cutánea más superficial. Comprender la relación entre estas afecciones, sus causas y las estrategias de tratamiento eficaces es crucial para controlar esta afección potencialmente mortal. Este artículo explorará la naturaleza del angioedema, su relación con la urticaria, los tratamientos disponibles y las medidas preventivas.

Comprender el angioedema
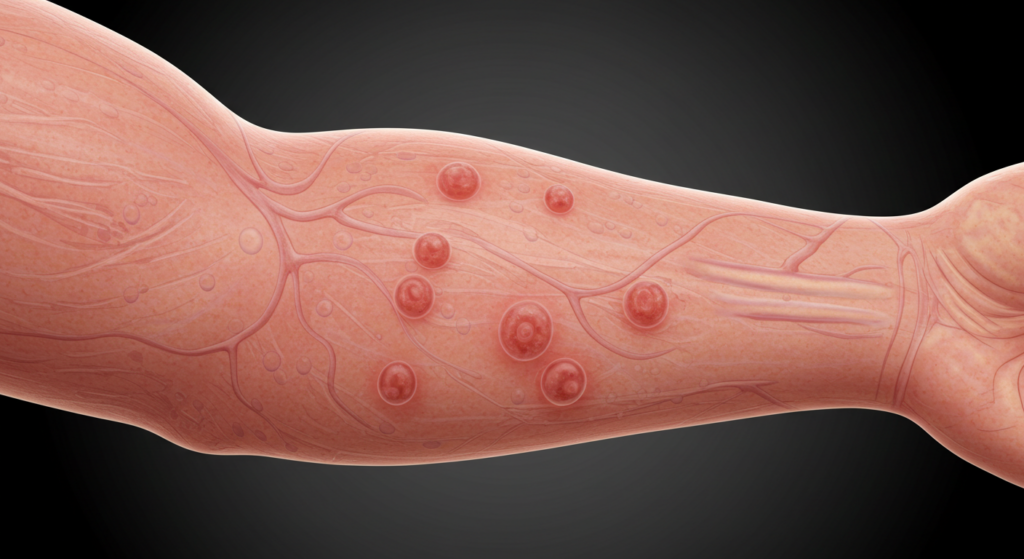
El angioedema se presenta como áreas extensas e hinchadas que generalmente afectan las capas más profundas de la piel. A diferencia de la urticaria, que consiste en ronchas elevadas que pican, el angioedema causa hinchazón que a menudo es indolora, pero puede ser muy incómoda. Las zonas comúnmente afectadas incluyen la cara, los labios, la lengua, las manos, los pies y los genitales. La hinchazón puede ser repentina y drástica, y aparecer en cuestión de minutos u horas. En casos graves, la hinchazón puede afectar las vías respiratorias, causando dificultad para respirar, una emergencia potencialmente mortal. La gravedad del angioedema varía considerablemente, desde una hinchazón leve y localizada hasta una reacción generalizada, potencialmente mortal. Es importante tener en cuenta que el angioedema puede presentarse independientemente de la urticaria o ser parte de una reacción alérgica más extensa.
La causa subyacente del angioedema suele ser una reacción alérgica desencadenada por diversos factores, como ciertos alimentos, medicamentos, picaduras de insectos o látex. Sin embargo, algunos casos no están relacionados con alergias. El angioedema hereditario (AEH) es un trastorno genético poco común que causa episodios recurrentes de inflamación debido a la deficiencia o disfunción de una proteína que regula la bradicinina, una molécula implicada en la inflamación. El angioedema adquirido es otro tipo de angioedema, que surge de diversas afecciones o medicamentos que afectan la regulación de la bradicinina. Un diagnóstico preciso es fundamental para determinar el tratamiento adecuado. A menudo es necesario realizar una historia clínica completa y una exploración física, junto con posibles pruebas de alergia y análisis de sangre.
Los síntomas del angioedema pueden variar según la zona afectada y la gravedad de la inflamación. En casos leves, la inflamación puede ser localizada y solo causar molestias. Sin embargo, los casos más graves pueden presentar una inflamación significativa de la cara, los labios y la lengua, lo que puede obstruir las vías respiratorias y causar dificultad para respirar. Otros síntomas pueden incluir dolor abdominal, náuseas, vómitos y diarrea, especialmente en casos que afectan el tracto gastrointestinal. La aparición repentina de inflamación, sobre todo en la cara o la garganta, requiere atención médica inmediata. Retrasar el tratamiento puede tener consecuencias graves.
El diagnóstico y el tratamiento oportunos son esenciales para prevenir complicaciones potencialmente mortales. Dado que el angioedema puede progresar rápidamente, requiere una intervención médica inmediata. Retrasar el tratamiento, especialmente en casos con compromiso de las vías respiratorias, puede provocar dificultad respiratoria grave e incluso la muerte. La rapidez de aparición y la posibilidad de una rápida intensificación de los síntomas subrayan la importancia de buscar atención médica inmediata ante cualquier signo de angioedema.

Angioedema y urticaria: el vínculo
El angioedema y la urticaria son reacciones cutáneas que implican inflamación, pero difieren en su profundidad y apariencia. La urticaria consiste en ronchas elevadas y pruriginosas que aparecen en las capas superficiales de la piel, mientras que el angioedema afecta la dermis más profunda y los tejidos subcutáneos, provocando una inflamación más profunda y difusa. Si bien pueden presentarse de forma independiente, con frecuencia aparecen juntos, a menudo como parte de una reacción alérgica más amplia. Esta coexistencia es común porque ambas afecciones comparten mecanismos subyacentes similares, que implican principalmente la liberación de histamina y otros mediadores inflamatorios.
La aparición simultánea de urticaria y angioedema sugiere una respuesta inflamatoria más extensa. La presencia de urticaria suele indicar una reacción alérgica más amplia, lo que aumenta la probabilidad de que el angioedema afecte a tejidos más profundos. Sin embargo, es fundamental comprender que el angioedema puede presentarse sin urticaria, especialmente en casos de angioedema hereditario u otras causas no alérgicas. La presencia o ausencia de urticaria no determina necesariamente la gravedad ni el enfoque terapéutico del angioedema.
Los mecanismos inmunológicos subyacentes que desencadenan tanto la urticaria como el angioedema implican la activación de los mastocitos y la liberación de mediadores inflamatorios como la histamina, la bradicinina y las prostaglandinas. Estos mediadores causan vasodilatación y un aumento de la permeabilidad vascular, lo que provoca la fuga de líquido a los tejidos y la consiguiente inflamación. La gravedad de la reacción depende de la cantidad y el tipo de mediadores liberados, así como de la sensibilidad individual. Por lo tanto, incluso desencadenantes aparentemente menores pueden provocar una respuesta significativa en personas susceptibles.
Diferenciar el angioedema de otras afecciones que imitan sus síntomas es crucial para un tratamiento eficaz. Afecciones como la celulitis (infección bacteriana de la piel), las picaduras de insectos y ciertas enfermedades autoinmunes pueden presentar una inflamación similar. Una evaluación clínica exhaustiva es esencial para distinguir el angioedema de estas afecciones, ya que los enfoques de tratamiento difieren significativamente. Para un diagnóstico preciso, pueden ser necesarios una historia clínica detallada, una exploración física y, posiblemente, otras pruebas, como análisis de sangre o biopsias de piel.
Estrategias de tratamiento eficaces
El tratamiento del angioedema depende de la gravedad de la inflamación y la causa subyacente. En casos leves de angioedema asociado con urticaria, los antihistamínicos suelen proporcionar alivio. Estos medicamentos bloquean la acción de la histamina, reduciendo la inflamación y el picor. Sin embargo, los antihistamínicos pueden ser menos eficaces para el angioedema que para la urticaria sola, especialmente en casos causados por mecanismos no mediados por la histamina. Generalmente son más seguros para el uso a largo plazo, pero su eficacia puede ser limitada en episodios graves.
En casos más graves, o cuando los antihistamínicos son insuficientes, se pueden recetar corticosteroides. Estos potentes antiinflamatorios pueden ayudar a reducir la hinchazón y la inflamación con mayor eficacia que los antihistamínicos. Los corticosteroides suelen administrarse por vía oral o intravenosa, según la gravedad de la reacción. Sin embargo, su uso suele limitarse a tratamientos a corto plazo debido a sus posibles efectos secundarios. No son una solución a largo plazo, sino una herramienta para controlar los episodios agudos.
En situaciones potencialmente mortales, como la obstrucción de las vías respiratorias debido a la inflamación de la lengua o la garganta, es necesaria una intervención médica inmediata. Esta puede incluir la administración de epinefrina (adrenalina), un potente broncodilatador y vasoconstrictor, para revertir rápidamente los efectos de la reacción alérgica. En casos graves, podría requerirse una intubación endotraqueal o una traqueotomía para asegurar la vía aérea. La actuación rápida es crucial en estas situaciones para prevenir la muerte.
El tratamiento específico del angioedema hereditario (AEH) difiere del del angioedema alérgico. El AEH requiere un manejo especializado, que a menudo incluye medicamentos que inhiben la producción o la acción de la bradicinina, el principal mediador de esta afección. Estos medicamentos pueden prevenir o reducir la frecuencia y la gravedad de los ataques de angioedema. Esto resalta la importancia de un diagnóstico correcto para garantizar el tratamiento adecuado.
Manejo y prevención del angioedema
El manejo del angioedema implica identificar y evitar los desencadenantes, si es posible. Esto puede requerir llevar un registro detallado de los posibles desencadenantes, como alimentos, medicamentos o factores ambientales, para identificar los causantes específicos. Las pruebas de alergia pueden ayudar a identificar alérgenos específicos, lo que permite implementar estrategias de prevención informadas. Este enfoque proactivo puede reducir significativamente la frecuencia de futuros episodios. La atención cuidadosa a los posibles desencadenantes es fundamental para el manejo a largo plazo.
Para las personas con desencadenantes conocidos, la evitación es la medida preventiva más eficaz. Esto puede implicar cambios en la dieta, ajustes en la medicación o evitar ciertos entornos. Llevar un autoinyector de epinefrina (EpiPen) de emergencia es crucial para las personas con riesgo de reacciones graves, ya que permite un autotratamiento rápido en caso de emergencia. Esta medida proactiva puede salvar vidas en situaciones donde existe riesgo de compromiso de las vías respiratorias.
Las revisiones médicas periódicas con un alergólogo o inmunólogo son esenciales para las personas con angioedema recurrente. Estos especialistas pueden proporcionar un seguimiento continuo, ajustar los planes de tratamiento según sea necesario y ofrecer orientación sobre el manejo y la prevención de futuros episodios. También pueden ayudar a identificar las afecciones subyacentes que contribuyen al angioedema y brindar asesoramiento personalizado para su manejo. Este enfoque colaborativo es crucial para un manejo eficaz a largo plazo.
Además del tratamiento médico, las técnicas de reducción del estrés pueden ser beneficiosas. El estrés puede exacerbar las reacciones alérgicas y las respuestas inflamatorias, lo que podría aumentar el riesgo de ataques de angioedema. Técnicas como el yoga, la meditación o los ejercicios de respiración profunda pueden ayudar a controlar los niveles de estrés y promover el bienestar general. Este enfoque holístico para el manejo del angioedema puede mejorar significativamente la calidad de vida y reducir la frecuencia de los episodios.
El angioedema, aunque potencialmente grave, es una afección controlable con un diagnóstico y tratamiento adecuados. Comprender la relación entre el angioedema y la urticaria, reconocer las diversas causas e implementar estrategias de manejo eficaces es crucial para mejorar la calidad de vida de las personas afectadas. La atención médica inmediata es esencial en casos de inflamación grave, especialmente en las vías respiratorias, para prevenir complicaciones potencialmente mortales. Un enfoque colaborativo entre los profesionales de la salud y la persona afectada es clave para el éxito del manejo y la prevención del angioedema a largo plazo.
Descubra la experiencia de la Dra. Ebru Okyay, su médico de confianza. dermatólogo en AntalyaYa sea que esté buscando abordar problemas médicos de la piel o mejorar su belleza natural con tratamientos cosméticos, el Dr. Okyay está aquí para ayudarlo. Con atención personalizada y técnicas avanzadas, lograr sus objetivos para la piel nunca ha sido tan fácil.
