Are you living with vitiligo and wondering if surgery could be the right path to restoring your skin’s even tone? As a leading dermatologist in Antalya, Dr. Ebru Okyay understands the emotional and physical challenges of this autoimmune condition. Vitiligo affects millions worldwide, causing white patches on the skin due to melanin loss. While topical treatments and phototherapy are first-line options, surgery offers hope for stable cases. In this comprehensive 2025 guide, we’ll explore who qualifies as ideal vitiligo surgery candidates, the strict selection criteria, and what to expect for optimal results.
This article draws from the latest clinical guidelines and my extensive experience treating vitiligo patients at drebruokyay.com clinic. Whether you’re seeking depigmentation, skin grafting, or melanocyte transplantation, understanding candidacy is key to achieving natural-looking outcomes. Let’s dive into the essentials to help you determine if you’re a suitable candidate.
Understanding Vitiligo and When Surgery Becomes an Option
Vitiligo is a chronic skin disorder where the immune system attacks melanocytes, the cells responsible for pigment production. This leads to depigmented patches that can appear anywhere on the body, often starting on the face, hands, or feet. In 2025, advancements in dermatology have expanded treatment horizons, but surgery is typically reserved for cases where medical therapies fall short.
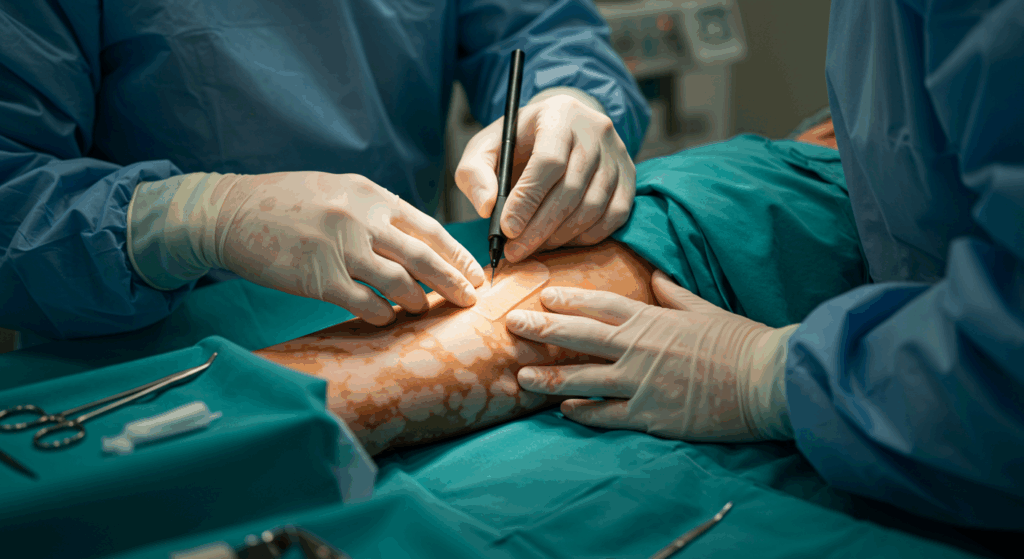
Surgical interventions for vitiligo aim to repigment affected areas or, in extensive cases, depigment the remaining skin for uniformity. Common procedures include tissue grafting, blister grafting, and cellular transplantation techniques like melanocyte-keratinocyte suspension. However, not everyone is eligible. Surgery is most effective for patients with stable vitiligo—meaning no new patches for at least 1-2 years—and localized lesions less than 50% of body surface area.

Types of Vitiligo and Their Surgical Suitability
Vitiligo manifests in various forms, each influencing surgical candidacy. Segmental vitiligo, which affects one side or segment of the body, responds well to surgery due to its stability. Non-segmental or generalized vitiligo, covering larger areas, may require a combination approach but is riskier for widespread procedures.
| Type of Vitiligo | Description | Surgical Suitability |
|---|---|---|
| Segmental Vitiligo | Affects a single dermatome; often stable after initial progression. | High – Ideal for localized grafting. |
| Non-Segmental Vitiligo | Symmetrical patches on both sides; progressive. | Moderate – Surgery for stable, focal areas only. |
| Universal Vitiligo | Affects over 80% of body surface; extensive depigmentation. | Low – Depigmentation surgery may be considered. |
| Focal Vitiligo | Limited to one or few small patches. | High – Excellent for cellular transplants. |
For more on vitiligo basics, check our Understanding the Basics of Vitiligo Surgery guide.
In my practice, I’ve seen surgery transform lives for patients with resistant patches on visible areas like the lips or eyelids, where camouflage is challenging. However, success hinges on precise patient selection to minimize recurrence and complications.
Key Selection Criteria for Vitiligo Surgery Candidates
Selecting the right vitiligo surgery candidates is both an art and a science. As per 2025 International Vitiligo Guidelines, criteria focus on disease stability, lesion characteristics, patient health, and psychological readiness. Let’s break down the essential factors that determine eligibility.
1. Disease Stability and Duration
The cornerstone of candidacy is stability. Active vitiligo, with spreading patches, contraindicates surgery as grafts can fail or trigger the Koebner phenomenon—new lesions at trauma sites. Ideal candidates have:
- No new or expanding lesions for at least 12-24 months.
- Disease duration of over 2 years, indicating burnout phase.
- Response to prior medical therapies like narrowband UVB, confirming stability.
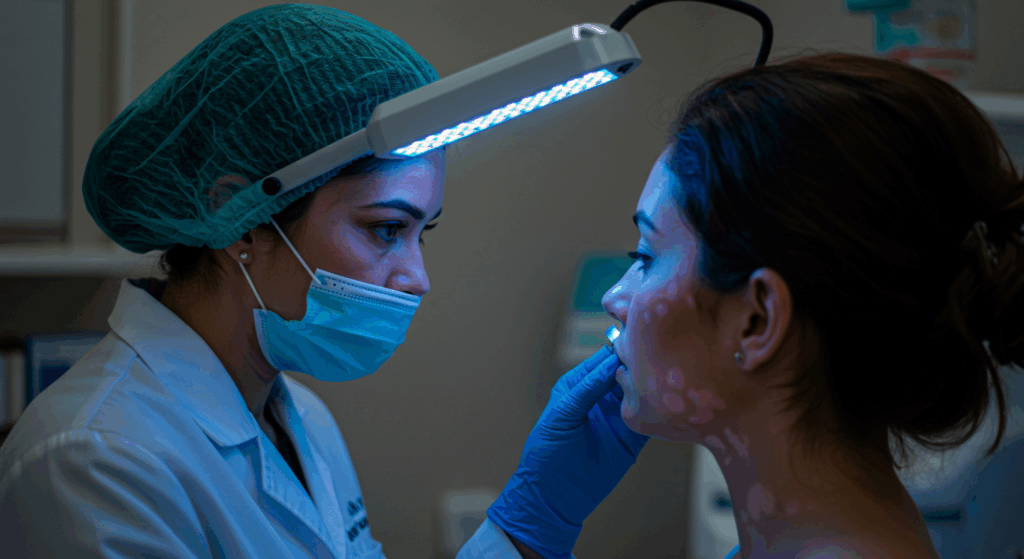
In my Antalya clinic, we use Wood’s lamp examinations and serial photography to verify stability over 6-12 months before proceeding.
2. Lesion Size, Location, and Characteristics
Not all vitiligo patches are surgical. Small, well-defined lesions (under 5 cm²) in cosmetically sensitive areas like the face or hands are prime targets. Achromic, follicular, or hypopigmented patches repigment better than lip or acral (hands/feet) sites, which have poorer blood supply.
| Lesion Location | Surgical Success Rate | Recommended Procedure |
|---|---|---|
| Face/Neck | 80-90% | Melanocyte suspension or blister grafting. |
| Trunk/Limbs | 70-85% | Tissue grafting for larger areas. |
| Hands/Feet | 50-70% | Limited to small, stable patches; cellular methods preferred. |
| Lips/Eyelids | 60-80% | Specialized micrografting techniques. |
Avoid surgery on unstable, confluent, or very large patches (>20 cm), as repigmentation rates drop below 50%.
3. Patient Age, Skin Type, and Health Status
Age plays a role: Adults over 18 with mature skin heal better, though adolescents with stable vitiligo may qualify under supervision. Fitzpatrick skin types I-III (lighter skin) show higher success, but types IV-VI can benefit with adjunct therapies.
Health criteria exclude candidates with:
- Active autoimmune diseases (e.g., thyroiditis, unless controlled).
- Known keloid scarring tendency.
- Uncontrolled diabetes, hypertension, or smoking history (increases failure risk by 30%).
- Pregnancy or breastfeeding (defer 6 months post).
Preoperative blood work, including thyroid function and vitamin D levels, is mandatory to rule out comorbidities.
4. Psychological and Lifestyle Factors
Surgery isn’t just physical; emotional readiness is crucial. Candidates must have realistic expectations—repigmentation is 70-90% at best, and recurrence possible in 20%. Those with body dysmorphic tendencies or high anxiety may need counseling first.
Lifestyle-wise, commitment to post-op care (sun protection, no trauma) is essential. In 2025, we emphasize shared decision-making, discussing alternatives like JAK inhibitors if surgery isn’t ideal.
Explore surgical techniques in detail via our Techniques and Methods in Vitiligo Surgery article.
Preoperative Assessment: Evaluating Your Candidacy
A thorough evaluation is the gateway to successful vitiligo surgery. At drebruokyay.com in Antalya, our process begins with a detailed consultation to assess all selection criteria.
Step-by-Step Preoperative Protocol
1. Medical History Review: Document vitiligo onset, progression, family history, and prior treatments. Screen for contraindications like immunosuppression.
2. Physical Examination: Use dermoscopy and UV light to map lesions, assess donor site viability (e.g., thigh for grafts), and evaluate skin laxity.
3. Photographic Documentation: Baseline images track stability over follow-ups.
4. Laboratory Tests: CBC, thyroid panel, HbA1c, and autoimmune markers ensure safety.
5. Psychological Screening: Brief assessments gauge motivation and coping mechanisms.
Advanced Diagnostic Tools in 2025
Modern tools enhance accuracy: Confocal microscopy visualizes melanocyte activity, while AI-assisted lesion mapping predicts repigmentation potential. These help tailor procedures, boosting success to 85% for qualified candidates.
| Assessment Step | Purpose | Expected Duration |
|---|---|---|
| History & Exam | Identify risks and stability | 30-45 minutes |
| Lab Tests | Rule out comorbidities | 1-2 weeks for results |
| Imaging/Dermoscopy | Lesion characterization | 20 minutes |
| Counseling | Set expectations | 45 minutes |
If assessments confirm candidacy, we proceed to planning. For indications, refer to our Vitiligo Surgery Indications Guide.
Risks, Outcomes, and Long-Term Management for Candidates
Even ideal vitiligo surgery candidates face risks, but informed choices mitigate them. Outcomes vary, with 70-95% repigmentation in facial lesions, per 2025 studies.
Potential Risks and How to Minimize Them
Common risks include infection (5%), scarring (10-15%), or partial graft failure (20%). In darker skin, hypopigmentation mismatches occur. We minimize via sterile techniques, antibiotics, and silicone sheets for scars.
- Perioperative Care: Strict hygiene and wound dressing.
- Adjunct Therapies: Post-op phototherapy enhances graft take.
- Follow-Up: Monthly checks for 6 months.
Expected Outcomes and Success Rates
Success is defined as >75% repigmentation at 1 year. Factors boosting rates: Stable disease, facial sites, and combined therapies. In my experience, 85% of candidates achieve satisfactory results, with color matching improving over 18 months.
| Procedure | Success Rate (% Repigmentation) | Ideal Candidate Profile |
|---|---|---|
| Skin Grafting | 70-85% | Small, stable patches on trunk. |
| Blister Grafting | 80-90% | Facial lesions; minimal donor morbidity. |
| Melanocyte Transplant | 75-95% | Large areas; good donor melanocytes. |
| Depigmentation | 90-100% uniformity | Extensive vitiligo (>50% BSA). |
Long-term, 10-20% experience recurrence, managed with maintenance UVB. See outcomes in our Outcomes and Success Rates of Vitiligo Surgery post.
Conclusion
Key Takeaways
- Ideal vitiligo surgery candidates have stable disease for 1-2 years, localized lesions, and no major health contraindications.
- Preoperative assessments including exams, labs, and counseling ensure safety and realistic expectations.
- Surgical outcomes reach 70-95% repigmentation, with risks minimized through expert care.
- In 2025, Antalya clinics like drebruokyay.com offer advanced, personalized vitiligo surgery for transformative results.
Next Steps
Considering vitiligo surgery? Start by:
- Tracking your lesions for stability over 6 months.
- Consulting a dermatologist for comprehensive evaluation.
- Schedule a free consultation at drebruokyay.com to discuss your candidacy.
- Explore non-surgical options if surgery isn’t suitable yet.
Dr. Ebru Okyay is dedicated to empowering vitiligo patients with evidence-based care in Antalya.
Frequently Asked Questions (FAQs)
Who is the ideal candidate for vitiligo surgery?
Ideal candidates have stable vitiligo for at least 12 months, localized patches, good health, and realistic expectations. Facial lesions often yield the best results.
How long must vitiligo be stable before surgery?
Typically 1-2 years without new patches. This reduces risks like Koebner phenomenon and improves graft survival.
What health conditions disqualify someone from vitiligo surgery?
Active infections, uncontrolled autoimmune diseases, clotting disorders, or keloid scarring history. Smoking cessation is required 4-6 weeks prior.
Is vitiligo surgery painful?
Local anesthesia ensures minimal discomfort during the procedure. Post-op soreness is managed with mild painkillers for 3-5 days.
What is the recovery time after vitiligo surgery?
Downtime is 7-14 days for wound healing. Full repigmentation takes 3-6 months, with restrictions on sun exposure and activities.
Can surgery cure vitiligo completely?
Surgery repigments specific areas but doesn’t cure the underlying autoimmune process. Recurrence is possible in 10-20% of cases.
Is vitiligo surgery suitable for children?
Rarely; only for adolescents over 16 with stable, focal vitiligo after failed medical therapy and parental consent.
How much does vitiligo surgery cost in Antalya?
Costs range from $2,000-$5,000 depending on procedure and lesion size. Consultations are complimentary at drebruokyay.com.
