Our skin, the largest organ in our body, acts as a vital barrier protecting us from the outside world. However, this protective shield is not impenetrable. It can be susceptible to various infections, and among the most common are fungal infections. These infections, caused by microscopic organisms called fungi, can affect various parts of the skin, causing discomfort, irritation, and sometimes, more serious complications if left untreated.
Understanding fungal skin infections is crucial for maintaining overall skin health and well-being. This comprehensive guide will delve into the world of fungal skin infections, exploring their causes, types, symptoms, treatments, and most importantly, preventative measures you can take to keep your skin healthy and fungus-free.
What are Fungal Skin Infections?
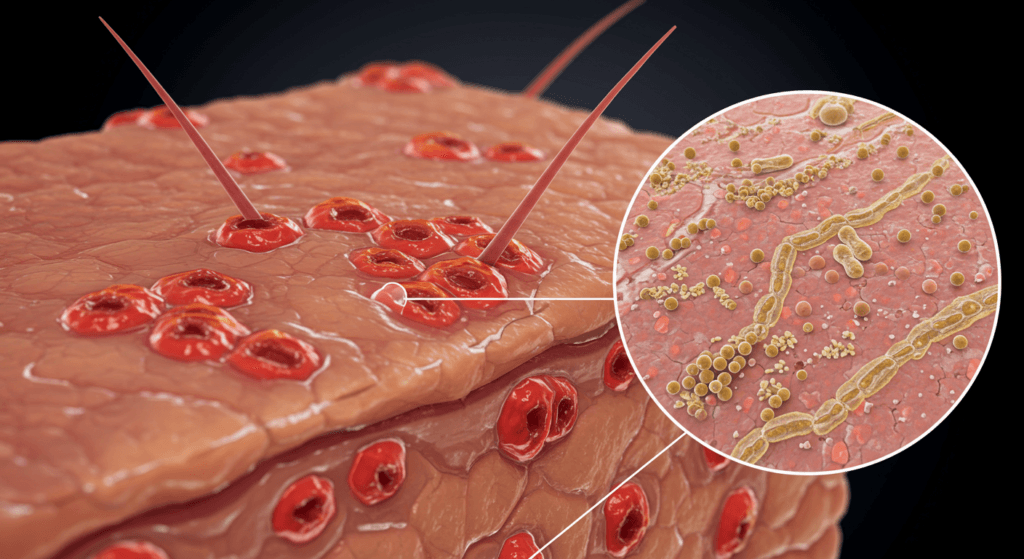
Fungal skin infections, also known as mycoses, are common conditions caused by parasitic microscopic organisms called fungi. These fungi thrive in warm, moist environments and can live on dead tissues of the hair, nails, and outer skin layers. While many types of fungi exist, only a small fraction are responsible for causing skin infections in humans.
These infections are not just a minor inconvenience; they can significantly impact your quality of life, causing itching, redness, scaling, and discomfort. In some cases, especially for individuals with weakened immune systems, fungal infections can become more severe and spread beyond the skin.
Types of Fungi that Cause Skin Infections
Several types of fungi can cause skin infections. The most common categories include:
- Dermatophytes: These are the most frequent culprits behind fungal skin infections. Dermatophytes are a group of fungi that thrive on keratin, a protein found in skin, hair, and nails. Infections caused by dermatophytes are often referred to as “tinea” infections, followed by the body part affected (e.g., tinea pedis for athlete’s foot). Common dermatophytes include Trichophyton, Microsporum, and Epidermophyton species.
- Yeasts: Yeasts are another type of fungus that can cause skin infections. Candida species are the most common yeasts responsible for skin infections, particularly Candida albicans. Candida infections are often found in moist areas of the body, such as the groin, armpits, and mouth. Malassezia is another type of yeast that can cause skin conditions like pityriasis versicolor (a skin discoloration condition) and seborrheic dermatitis (a common skin condition causing scaly patches and dandruff).
- Molds: While less common than dermatophytes and yeasts, certain molds can also cause skin infections, especially in individuals with compromised immune systems.
Conditions that Favor Fungal Growth
Fungi thrive in specific conditions, making certain environments and habits more conducive to fungal skin infections. These favorable conditions include:
- Warmth and Moisture: Fungi flourish in warm, humid environments. Areas of the body that tend to trap moisture, such as sweaty feet, groin folds, and areas under skin folds, are particularly vulnerable.
- Poor Hygiene: Inadequate hygiene practices, such as infrequent washing, not drying skin thoroughly after bathing, and wearing damp clothing, can create a breeding ground for fungi.
- Weakened Immune System: Individuals with weakened immune systems, due to conditions like HIV/AIDS, diabetes, or immunosuppressant medications, are more susceptible to fungal infections as their bodies are less able to fight off fungal overgrowth.
- Tight Clothing and Footwear: Wearing tight, non-breathable clothing and footwear can trap moisture and heat against the skin, creating an ideal environment for fungal growth.
- Contact with Infected Individuals or Animals: Fungal infections can be contagious and spread through direct contact with infected individuals, animals, or contaminated surfaces.
- Certain Medical Conditions: Conditions like diabetes and obesity can increase the risk of fungal infections due to factors like impaired circulation, skin folds, and weakened immune response.
Common Types of Fungal Skin Infections
Fungal skin infections can manifest in various forms, depending on the type of fungus involved and the area of the body affected. Here are some of the most common types:
- Athlete’s Foot (Tinea Pedis): This is one of the most prevalent fungal skin infections, typically affecting the feet, particularly between the toes. It’s often characterized by itching, burning, stinging, redness, scaling, and cracking skin. Athlete’s foot is highly contagious and commonly spread in damp environments like swimming pools, locker rooms, and showers.
- Ringworm (Tinea Corporis, Tinea Cruris, Tinea Capitis): Despite its name, ringworm is not caused by worms but by dermatophyte fungi. It manifests as circular, raised, scaly, and itchy rashes that often have a ring-like appearance. Ringworm can affect various parts of the body:
- Tinea Corporis: Ringworm of the body, occurring on the trunk, arms, or legs.
- Tinea Cruris (Jock Itch): Ringworm in the groin area, common in athletes and individuals who wear tight clothing.
- Tinea Capitis: Ringworm of the scalp, primarily affecting children and causing scaly patches, hair loss, and sometimes inflammation.
- Yeast Infections (Cutaneous Candidiasis): These infections are caused by Candida yeasts and typically occur in moist areas like skin folds, groin, armpits, and under the breasts. Symptoms include redness, itching, burning, and a creamy white discharge. Oral thrush (candidiasis in the mouth) and vaginal yeast infections are also common forms of Candida infections.
- Nail Fungus (Onychomycosis): Nail fungus affects the nails, usually toenails, causing thickening, discoloration (yellowish or whitish), brittleness, and sometimes pain or discomfort. Nail fungus infections are often persistent and can be challenging to treat.
- Pityriasis Versicolor (Tinea Versicolor): This fungal infection, caused by Malassezia yeast, results in patches of discolored skin, typically on the trunk, neck, and upper arms. The patches can be lighter or darker than the surrounding skin and may become more noticeable in the summer.
- Seborrheic Dermatitis: While not solely a fungal infection, Malassezia yeast plays a significant role in seborrheic dermatitis, a common inflammatory skin condition causing scaly, flaky, and itchy patches, often on the scalp (dandruff), face, and chest.
Symptoms of Fungal Skin Infections
The symptoms of fungal skin infections can vary depending on the type of infection and the area affected. However, some common symptoms to watch out for include:
- Itching: Persistent itching is a hallmark symptom of many fungal skin infections. The itching can range from mild to intense and may worsen with scratching.
- Redness: The affected skin area often becomes red and inflamed.
- Scaling or Flaking: The skin may become dry, scaly, and flaky, with peeling or cracking.
- Burning or Stinging: A burning or stinging sensation, especially in areas like the feet or groin, is common in athlete’s foot and jock itch.
- Rashes: Fungal infections often present as rashes that can be circular, ring-shaped, or irregular.
- Blisters or Vesicles: Small blisters or fluid-filled vesicles may develop in some fungal infections, particularly athlete’s foot.
- Discoloration: Pityriasis versicolor causes patches of skin discoloration, which can be lighter or darker than the surrounding skin. Nail fungus can cause nail discoloration (yellowish or whitish).
- Thickening or Brittleness of Nails: Nail fungus leads to thickening, brittleness, and changes in nail texture.
- Hair Loss (in Tinea Capitis): Ringworm of the scalp can cause patches of hair loss, often accompanied by scaling and inflammation.
It’s important to note that these symptoms can also be associated with other skin conditions. Therefore, it’s crucial to consult a dermatologist for proper diagnosis and treatment if you suspect a fungal skin infection.
Causes and Risk Factors for Fungal Skin Infections
Understanding the causes and risk factors for fungal skin infections can help you take preventative measures. Key factors contributing to these infections include:
- Exposure to Fungi: Direct contact with fungi is the primary cause of fungal skin infections. This can occur through:
- Contact with Infected Individuals or Animals: Sharing personal items like towels, clothing, or shoes with an infected person, or touching infected pets can spread fungi.
- Contaminated Surfaces: Walking barefoot in public places like swimming pools, locker rooms, showers, and gyms exposes your feet to fungi present on these surfaces.
- Soil and Plants: Some fungi live in soil and on plants, and direct contact can lead to infections, particularly for gardeners or outdoor enthusiasts.
- Environmental Factors:
- Warm and Humid Climates: Hot and humid weather promotes fungal growth and increases the risk of infections.
- Sweating: Excessive sweating, especially in enclosed areas like feet and groin, creates a moist environment favorable for fungi.
- Hygiene Practices:
- Poor Hygiene: Infrequent bathing or showering, not drying skin thoroughly, and wearing unclean clothing can increase the risk.
- Sharing Personal Items: Sharing towels, razors, socks, shoes, and other personal items can facilitate fungal transmission.
- Lifestyle Factors:
- Tight Clothing and Footwear: Wearing tight, non-breathable clothing and shoes traps moisture and heat, promoting fungal growth.
- Athletic Activities: Athletes are at higher risk due to increased sweating, shared locker rooms, and frequent use of public showers.
- Medical Conditions and Medications:
- Weakened Immune System: Conditions like HIV/AIDS, diabetes, autoimmune diseases, and medications that suppress the immune system (e.g., corticosteroids, chemotherapy) increase susceptibility to fungal infections.
- Antibiotic Use: Antibiotics can disrupt the natural balance of microorganisms on the skin, potentially allowing fungi to overgrow.
- Obesity: Skin folds in obese individuals can trap moisture and create a favorable environment for fungal infections.
- Diabetes: Individuals with diabetes are more prone to infections, including fungal infections, due to impaired circulation and immune function.
- Age: Both very young children and older adults may be more susceptible to certain fungal infections.
Diagnosis of Fungal Skin Infections
Accurate diagnosis is essential for effective treatment of fungal skin infections. A dermatologist can typically diagnose a fungal skin infection through:
- Physical Examination: The dermatologist will visually examine the affected skin, noting the appearance, location, and distribution of the rash or lesions. The pattern and characteristics of the rash often provide clues to the type of fungal infection.
- Medical History: The dermatologist will inquire about your medical history, including any pre-existing conditions, medications, lifestyle factors, and potential exposures that might contribute to the infection.
- Skin Scraping (KOH Preparation): This is a common and quick diagnostic test. The dermatologist will gently scrape a small sample of skin scales from the affected area. The scraping is then placed on a microscope slide with potassium hydroxide (KOH) solution. KOH dissolves skin cells, making fungal elements (hyphae or spores) more visible under a microscope. This test can quickly confirm the presence of fungi.
- Fungal Culture: In some cases, a fungal culture may be necessary, especially if the diagnosis is uncertain or if the infection is severe or recurrent. A skin scraping or nail clipping is collected and sent to a laboratory to grow the fungus in a culture medium. This allows for identification of the specific type of fungus causing the infection, which can guide treatment decisions, particularly for resistant infections.
- Skin Biopsy (Rarely Needed): In rare, complex, or atypical cases, a skin biopsy may be performed. A small skin sample is removed and examined under a microscope to rule out other conditions and confirm the fungal infection.
Treatment Options for Fungal Skin Infections
Treatment for fungal skin infections depends on the type and severity of the infection. Options range from over-the-counter (OTC) medications to prescription antifungal drugs:
- Over-the-Counter (OTC) Antifungal Medications: For mild to moderate fungal skin infections like athlete’s foot, jock itch, and ringworm, OTC antifungal creams, lotions, sprays, and powders are often effective. Common OTC antifungal ingredients include:
- Clotrimazole
- Miconazole
- Terbinafine
- Tolnaftate
- Undecylenate
- Prescription Antifungal Medications: For more severe, widespread, or persistent fungal infections, or for nail fungus and scalp ringworm, prescription antifungal medications are often necessary. These medications are stronger and more effective than OTC options and may be prescribed in topical or oral forms:
- Topical Prescription Antifungals: Stronger antifungal creams and ointments containing ingredients like ketoconazole, econazole, ciclopirox, and nystatin may be prescribed for skin infections.
- Oral Antifungal Medications: For nail fungus, scalp ringworm, and severe skin infections, oral antifungal medications are often required. Common oral antifungals include terbinafine, itraconazole, fluconazole, and griseofulvin. Oral antifungal medications are taken by mouth and work systemically to fight the infection. They typically require a longer course of treatment (weeks to months) and may have potential side effects, so regular monitoring by a physician is important.
- Prescription Antifungal Shampoos and Washes: For scalp ringworm and seborrheic dermatitis, prescription antifungal shampoos containing ketoconazole, selenium sulfide, or ciclopirox may be prescribed to help control fungal overgrowth and reduce symptoms. Antifungal washes may also be prescribed for body infections.
- Home Remedies and Supportive Measures: While home remedies alone may not cure fungal infections, they can provide symptom relief and support treatment:
- Good Hygiene: Maintain good hygiene by washing the affected area daily with soap and water, and drying thoroughly, especially in skin folds.
- Keep Skin Dry and Cool: Wear loose-fitting, breathable clothing, and change out of sweaty clothes promptly. Use absorbent powders (like talcum powder, if tolerated) in areas prone to moisture.
- Avoid Irritants: Avoid harsh soaps, detergents, and perfumes that can irritate the skin and worsen symptoms.
- Cool Compresses: Cool compresses can help soothe itching and inflammation.
- Soaking Feet (for Athlete’s Foot): Soaking feet in salt water or diluted vinegar solution may help dry out blisters and relieve itching in athlete’s foot.
It’s crucial to consult a dermatologist for proper diagnosis and treatment of fungal skin infections. Self-treating with OTC medications for prolonged periods or for severe infections can delay appropriate care and potentially lead to complications or recurrence. A dermatologist can accurately diagnose the type of fungal infection, recommend the most effective treatment plan, and monitor your progress.
Prevention of Fungal Skin Infections: Proactive Steps for Healthy Skin
Prevention is always better than cure. Adopting preventative measures can significantly reduce your risk of developing fungal skin infections:
- Practice Good Hygiene:
- Shower or Bathe Regularly: Wash your body daily with soap and water, especially after sweating or exercising.
- Dry Skin Thoroughly: Pay particular attention to drying skin folds, between toes, and groin area after bathing or swimming.
- Wash Hands Frequently: Wash your hands thoroughly and frequently, especially after being in public places or touching potentially contaminated surfaces.
- Keep Skin Dry and Cool:
- Wear Loose-Fitting, Breathable Clothing: Choose clothing made of cotton or other breathable fabrics that wick away moisture. Avoid tight-fitting synthetic clothing.
- Wear Breathable Footwear: Opt for shoes made of breathable materials like leather or canvas, and alternate shoes to allow them to dry out completely between wearings.
- Use Absorbent Powder: Apply absorbent powder (like talcum powder, if tolerated) to areas prone to sweating, such as feet and groin, to help keep them dry.
- Avoid Sharing Personal Items:
- Don’t Share Towels, Clothing, or Shoes: Avoid sharing personal items that can harbor fungi, such as towels, clothing, socks, shoes, razors, and nail clippers.
- Use Your Own Personal Care Products: Use your own soaps, shampoos, and personal care products.
- Protect Your Feet in Public Places:
- Wear Shower Shoes or Sandals in Public Showers, Locker Rooms, and Swimming Pools: Avoid walking barefoot in these damp public areas to minimize exposure to fungi.
- Maintain a Healthy Immune System:
- Eat a Balanced Diet: Consume a nutritious diet rich in fruits, vegetables, and whole grains to support a strong immune system.
- Get Enough Sleep: Adequate sleep is essential for immune function.
- Manage Stress: Chronic stress can weaken the immune system. Practice stress-reducing techniques like exercise, yoga, or meditation.
- Manage Underlying Medical Conditions: Effectively manage conditions like diabetes and HIV/AIDS to optimize immune function.
- Proper Nail Care:
- Keep Nails Clean and Dry: Keep fingernails and toenails clean and dry.
- Avoid Nail Trauma: Prevent nail injuries, as damaged nails are more susceptible to fungal infections.
- Use Clean Nail Tools: Use clean and disinfected nail clippers and files.
- Treat Existing Infections Promptly: If you develop a fungal skin infection, seek prompt treatment to prevent it from spreading to other areas of your body or to other people.
When to See a Dermatologist for Fungal Skin Infections
While mild fungal skin infections may respond to OTC treatments, it’s important to know when to seek professional medical help from a dermatologist. Consult a dermatologist if:
- Symptoms are Severe or Worsening: If your symptoms are intense, rapidly worsening, or not improving with OTC treatments within a week or two.
- Infection is Widespread: If the infection covers a large area of your body.
- Infection Affects Nails or Scalp: Nail fungus and scalp ringworm typically require prescription medications and dermatologist care.
- You Have a Weakened Immune System: Individuals with compromised immune systems should seek prompt medical attention for any suspected fungal infection.
- You Have Diabetes: People with diabetes are at higher risk for complications from infections and should seek professional care.
- Diagnosis is Uncertain: If you are unsure if you have a fungal infection or if your symptoms could be due to another skin condition, a dermatologist can provide accurate diagnosis.
- Recurrent Infections: If you experience frequent or recurring fungal skin infections, a dermatologist can help identify underlying factors and develop a preventative strategy.
- OTC Treatments are Ineffective: If OTC antifungal medications are not providing relief or clearing the infection after a reasonable trial period.
The Link Between Fungal Infections and Overall Skin Health
Fungal infections, while often perceived as minor skin issues, are intrinsically linked to overall skin health. Untreated or recurrent fungal infections can lead to:
- Chronic Skin Irritation and Discomfort: Persistent itching, redness, and scaling can significantly impact comfort and quality of life.
- Skin Damage and Secondary Infections: Scratching intensely to relieve itching can damage the skin barrier, increasing the risk of secondary bacterial infections.
- Spread of Infection: Fungal infections can spread to other parts of the body, including nails, scalp, and even internally in severe cases (especially in immunocompromised individuals).
- Discoloration and Scarring: Some fungal infections, like pityriasis versicolor, can cause skin discoloration. Severe or untreated infections can potentially lead to scarring.
- Impact on Self-Esteem and Social Well-being: Visible skin conditions, including fungal infections, can impact self-esteem and social interactions, particularly if they are widespread or affect visible areas like the face or hands.
Therefore, addressing fungal infections promptly and effectively is not just about relieving immediate symptoms; it’s also about safeguarding long-term skin health and overall well-being.
Conclusion: Proactive Skin Health and Fungal Infection Management
Fungal skin infections are common, but they are also often preventable and treatable. By understanding the causes, types, symptoms, and preventative measures, you can take proactive steps to protect your skin health and minimize your risk of fungal infections.
Maintaining good hygiene, keeping skin dry and cool, avoiding sharing personal items, and protecting your feet in public places are key preventative strategies. If you suspect you have a fungal skin infection, don’t hesitate to seek diagnosis and treatment from a dermatologist. With proper care and management, you can effectively address fungal skin infections and maintain healthy, comfortable, and beautiful skin. Remember, your skin is your body’s first line of defense – taking care of it is an investment in your overall health and well-being.
Discover the expertise of Dr. Ebru Okyay, your trusted dermatologist in Antalya. Whether you’re looking to address medical skin concerns or enhance your natural beauty with cosmetic treatments, Dr. Okyay is here to help. With personalized care and advanced techniques, achieving your skin goals has never been easier.
