Skin cancer is the most common type of cancer worldwide, affecting millions of people each year. While the diagnosis can be daunting, the good news is that skin cancer is often highly treatable, especially when detected early. Surgery remains a cornerstone of skin cancer treatment, offering effective solutions for various types and stages of the disease. This comprehensive overview will guide you through the different surgical options available for skin cancer, helping you understand your choices and what to expect.
Understanding Skin Cancer and the Role of Surgery
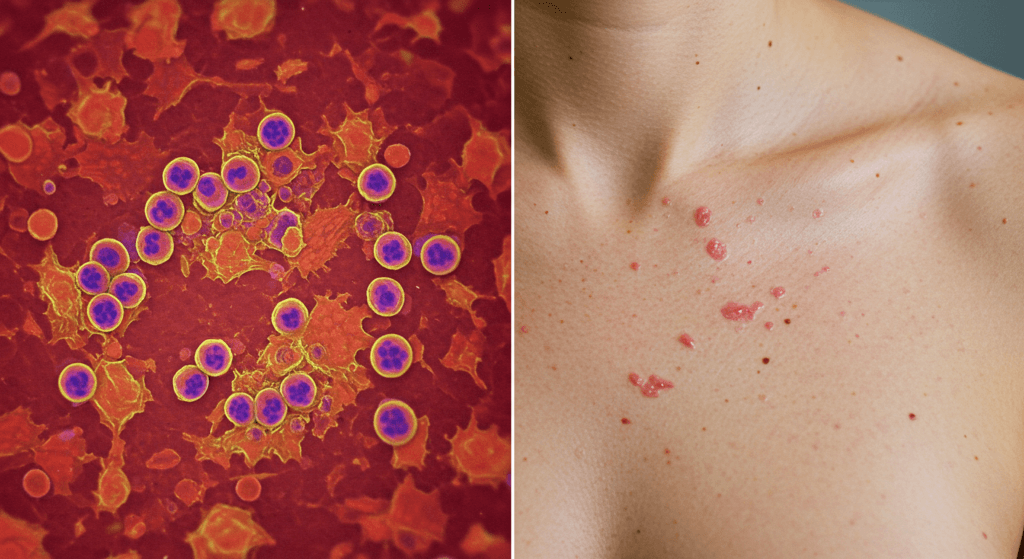
Before diving into surgical options, it’s crucial to understand what skin cancer is and why surgery is often the primary treatment. Skin cancer arises from the uncontrolled growth of abnormal skin cells. The most common types include:
- Basal Cell Carcinoma (BCC): The most frequent type, typically slow-growing and rarely metastasizes (spreads to other parts of the body).
- Squamous Cell Carcinoma (SCC): Also common, SCC has a slightly higher risk of metastasis than BCC, especially in certain locations or with specific characteristics.
- Melanoma: The most dangerous type of skin cancer due to its higher propensity to metastasize. Early detection and treatment are critical for melanoma.
Surgery plays a vital role in skin cancer treatment for several reasons:
- Removal of Cancerous Tissue: Surgery aims to physically remove the cancerous cells and a margin of surrounding healthy tissue to ensure complete eradication of the tumor.
- High Cure Rates: For many types and early stages of skin cancer, surgery offers excellent cure rates, often exceeding 90% when performed effectively.
- Definitive Treatment: In many cases, surgery can be the only treatment needed, eliminating the need for further therapies like radiation or chemotherapy, especially for early-stage BCCs and SCCs.
- Pathological Examination: Surgically removed tissue is sent to a pathologist for microscopic examination. This confirms the diagnosis, determines the type and grade of cancer, and ensures clear margins (meaning no cancer cells are detected at the edges of the removed tissue).
While surgery is highly effective, the best approach depends on several factors, including the type, size, location, and stage of the skin cancer, as well as your overall health and preferences. Let’s explore the main surgical options available.

Types of Skin Cancer Surgery: A Detailed Look
Several surgical techniques are employed to treat skin cancer, each with its own advantages and suitability depending on the specific situation.
1. Excisional Surgery: The Standard Approach
Excisional surgery is the most common and straightforward surgical method for treating skin cancer. It involves cutting out the visible tumor along with a margin of surrounding normal-appearing skin. This margin is crucial to ensure that any microscopic cancer cells extending beyond the visible tumor are also removed.
How it’s performed:
- Local Anesthesia: Typically, excisional surgery is performed under local anesthesia, meaning you’ll be awake but the area around the tumor will be numbed with an injection. In some cases, for larger or more complex excisions, general anesthesia might be considered.
- Excision: The surgeon uses a scalpel to carefully cut out the tumor and the predetermined margin of healthy tissue. The size of the margin depends on the type and size of the skin cancer and may range from a few millimeters to a centimeter or more.
- Closure: Once the tumor is removed, the wound is closed. The method of closure depends on the size and location of the excision.
- Direct Closure (Primary Closure): If the wound is small enough, the edges of the skin can be directly stitched together using sutures (stitches).
- Skin Flap or Graft: For larger excisions, especially in cosmetically sensitive areas, a skin flap (moving adjacent skin to cover the defect) or a skin graft (taking skin from another area of the body to cover the defect) may be necessary to achieve optimal cosmetic results.
- Pathology: The removed tissue is sent to a pathology lab for microscopic examination to confirm complete removal of the cancer and assess margins.
When is Excisional Surgery Used?
Excisional surgery is suitable for most types of skin cancer, including:
- Basal Cell Carcinoma (BCC): Effective for most BCCs, especially smaller, well-defined tumors.
- Squamous Cell Carcinoma (SCC): Often the first-line treatment for SCCs, particularly those that are not high-risk.
- Melanoma: Used for initial removal of melanomas. The margin of healthy tissue removed will be wider for melanoma compared to BCC or SCC, based on the melanoma’s thickness.
- Precancerous Lesions: Excisional surgery can also be used to remove certain precancerous lesions like actinic keratoses (if they are thick or concerning) or atypical moles.
What to Expect During and After Excisional Surgery:
- During Surgery: You will feel minimal discomfort thanks to the local anesthesia. You might feel some pressure or tugging during the procedure. The surgery itself typically takes 30 minutes to an hour, depending on the size and complexity.
- Immediately After Surgery: You will have a dressing over the wound. You may experience some mild pain or discomfort, which can be managed with over-the-counter pain relievers.
- Recovery: Recovery is generally straightforward. You’ll need to keep the wound clean and dry, following your surgeon’s instructions for wound care. Sutures are usually removed within 5-14 days, depending on the location and type of sutures used.
- Scarring: Excisional surgery will result in a scar. The size and appearance of the scar depend on the size and location of the excision, as well as individual healing factors. Scars typically fade over time.
Potential Risks and Complications:
Excisional surgery is generally safe, but potential risks and complications include:
- Bleeding: Minor bleeding is common immediately after surgery.
- Infection: Although rare with proper wound care, infection is a possibility.
- Scarring: Scarring is inevitable, but its appearance can vary.
- Nerve Damage: Rare, but possible, especially in areas with many superficial nerves.
- Recurrence: Although the goal is complete removal, there’s a small chance of cancer recurrence at the surgical site. Regular follow-up appointments are crucial for monitoring.
2. Mohs Surgery: Precision and Tissue Sparing
Mohs micrographic surgery is a highly specialized surgical technique considered the gold standard for treating certain types of skin cancer, particularly BCCs and SCCs in cosmetically sensitive areas or those with a higher risk of recurrence. Mohs surgery offers the highest cure rates for these cancers while minimizing the removal of healthy tissue.
How Mohs Surgery Works: Layer-by-Layer Removal and Examination
Mohs surgery is unique because it combines surgical removal with immediate microscopic examination of the tissue margins. This allows the surgeon to precisely map out and remove the cancer layer by layer, ensuring complete removal while preserving as much healthy skin as possible.
The Step-by-Step Mohs Process:
- Tumor Removal and Mapping: The surgeon removes the visible skin cancer and a thin layer of surrounding tissue. This layer is carefully mapped and marked to maintain its orientation.
- Microscopic Examination: The removed tissue layer is processed and examined under a microscope by the Mohs surgeon (who is specially trained in both surgery and pathology). The surgeon meticulously checks 100% of the surgical margin to see if any cancer cells remain.
- Repeat Layers (if needed): If cancer cells are found at the margin in a specific area, the surgeon returns to the patient and removes another thin layer of tissue only from that precise area, guided by the map. This process of removal and microscopic examination is repeated layer by layer until no cancer cells are detected at the margins.
- Wound Closure: Once clear margins are achieved, the wound is closed. The closure method depends on the size and location of the defect and may involve direct closure, skin flap, or skin graft.
Ideal Candidates for Mohs Surgery:
Mohs surgery is particularly recommended for:
- Basal Cell Carcinoma (BCC) and Squamous Cell Carcinoma (SCC): Especially for:
- High-Risk Tumors: Large tumors, aggressive subtypes, recurrent tumors, tumors with poorly defined borders.
- Cosmetically Sensitive Areas: Face (especially around the eyes, nose, lips, ears), neck, hands, and feet, where tissue preservation is crucial for appearance and function.
- Tumors in Scarred Areas or Areas of Prior Radiation: These tumors may have deeper roots and are more challenging to treat with standard excision.
- Rapidly Growing Tumors: Tumors that have grown quickly may be more aggressive.
Advantages of Mohs Surgery:
- Highest Cure Rates: Mohs surgery boasts the highest cure rates for BCC and SCC, often exceeding 99% for primary tumors and 95% for recurrent tumors.
- Tissue Sparing: By removing tissue layer by layer and examining 100% of the margins, Mohs surgery minimizes the removal of healthy skin, resulting in smaller scars and better cosmetic outcomes, especially in visible areas.
- Precise Margin Control: The microscopic examination during surgery ensures that all cancer cells are removed, reducing the risk of recurrence.
- Outpatient Procedure: Mohs surgery is typically performed in an outpatient setting under local anesthesia.
Recovery and Aftercare after Mohs Surgery:
- Wound Care: Similar to excisional surgery, meticulous wound care is essential. You will receive detailed instructions on cleaning the wound, applying ointment, and changing dressings.
- Healing Time: Healing time varies depending on the size and location of the wound, but it generally takes several weeks.
- Scarring: Mohs surgery aims to minimize scarring, but some scarring is expected. The appearance of the scar will improve over time.
- Follow-up: Regular follow-up appointments are necessary to monitor for any recurrence and for routine skin checks.
Potential Risks and Complications of Mohs Surgery:
Mohs surgery is generally safe, but potential risks are similar to excisional surgery, including bleeding, infection, scarring, and rare nerve damage. However, the risk of recurrence is significantly lower with Mohs surgery for appropriate tumors.
3. Curettage and Electrodesiccation (C&E): A Simpler Approach for Superficial Cancers
Curettage and electrodesiccation (C&E) is a simpler surgical technique primarily used for treating small, superficial basal cell carcinomas and precancerous lesions. It’s a quicker and less invasive option compared to excision or Mohs surgery.
How C&E is Performed:
- Local Anesthesia: The area is numbed with local anesthesia.
- Curettage: The surgeon uses a curette, a sharp, spoon-shaped instrument, to scrape away the cancerous tissue. Because cancer cells are typically softer than normal skin cells, the curette can selectively remove the tumor.
- Electrodesiccation: After curettage, electrodesiccation is performed. This involves using an electric current to cauterize (destroy) any remaining cancer cells at the base and edges of the treated area. This also helps to control bleeding.
- Wound Healing: The wound is left to heal naturally, without stitches. It typically heals like a scrape or abrasion.
When is C&E Appropriate?
C&E is best suited for:
- Small, Superficial Basal Cell Carcinomas (BCCs): Especially those on the trunk, arms, or legs that are not in high-risk locations and are well-defined.
- Precancerous Lesions (Actinic Keratoses): C&E can be an effective way to remove actinic keratoses.
- Superficial Squamous Cell Carcinomas (SCCs) in select cases: C&E may be considered for very small, low-risk SCCs in certain locations, but it’s less commonly used for SCCs compared to BCCs.
Advantages of C&E:
- Quick and Simple: C&E is a relatively quick and straightforward procedure, often taking only 15-30 minutes.
- Less Invasive: It’s less invasive than excisional surgery or Mohs surgery, resulting in a smaller wound and faster healing time.
- Cost-Effective: C&E is generally less expensive than other surgical options.
- No Sutures: The wound heals without stitches, simplifying aftercare.
Recovery and Aftercare after C&E:
- Wound Care: Keep the wound clean and dry. You may be instructed to apply a topical antibiotic ointment and a bandage.
- Healing Time: The wound typically heals within a few weeks, similar to a scrape.
- Scarring: C&E usually results in a round, slightly lighter scar that may be slightly depressed compared to the surrounding skin.
Limitations and When C&E is Not Suitable:
- Not for Aggressive or Deep Cancers: C&E is not appropriate for aggressive or deeply invasive skin cancers, melanomas, or tumors in high-risk locations.
- Margin Control: C&E does not offer the same level of margin control as Mohs surgery, as the tissue margins are not microscopically examined during the procedure.
- Recurrence Rate: The recurrence rate for C&E may be slightly higher than for Mohs surgery, especially for larger or more aggressive tumors.
4. Cryosurgery: Freezing Away Cancer Cells
Cryosurgery, also known as cryotherapy, uses extreme cold to freeze and destroy abnormal tissue, including skin cancer cells. Liquid nitrogen is the most common freezing agent used in cryosurgery.
How Cryosurgery is Performed:
- Freezing: Liquid nitrogen is applied directly to the skin cancer lesion using a spray device or a cotton-tipped applicator. The freezing process typically involves one or two freeze-thaw cycles, where the tissue is frozen and then allowed to thaw naturally.
- Cell Destruction: The freezing temperatures destroy the cancer cells.
- Wound Healing: After thawing, the treated area will blister, and eventually, a scab will form. The scab will fall off within a few weeks, and the underlying skin will heal.
When is Cryosurgery Used?
Cryosurgery is primarily used for:
- Precancerous Lesions (Actinic Keratoses): Cryosurgery is a very common and effective treatment for actinic keratoses.
- Small, Superficial Basal Cell Carcinomas (BCCs): Suitable for small, well-defined, superficial BCCs, especially in areas where cosmetic outcome is less of a concern (e.g., trunk, arms, legs).
- Superficial Squamous Cell Carcinomas (SCCs) in select cases: Less common for SCCs, but may be considered for very small, low-risk SCCs in certain situations.
- Lentigo Maligna (Melanoma in situ): Cryosurgery may be used in some cases of lentigo maligna, a type of melanoma that is confined to the epidermis (outer layer of skin).
Advantages of Cryosurgery:
- Quick and Convenient: Cryosurgery is a fast and relatively simple procedure that can be performed in a doctor’s office.
- No Cutting or Sutures: It’s a non-invasive technique that doesn’t involve cutting or stitches.
- Minimal Scarring (in some cases): Cryosurgery can sometimes result in less scarring than excisional surgery, although it can cause pigment changes (lighter or darker skin).
- Cost-Effective: Cryosurgery is generally less expensive than other surgical options.
Recovery and Aftercare after Cryosurgery:
- Blistering and Scabbing: Expect blistering and scabbing in the treated area, which is a normal part of the healing process.
- Wound Care: Keep the area clean and dry. You may be advised to apply a bandage.
- Healing Time: Healing typically takes several weeks, depending on the size and depth of the treated area.
- Pigment Changes: Cryosurgery can sometimes cause permanent pigment changes in the treated skin, resulting in lighter or darker patches.
Disadvantages and When Cryosurgery is Not Suitable:
- Less Precise Margin Control: Cryosurgery does not offer precise margin control, as the depth and extent of freezing can be difficult to control exactly.
- Not for Invasive Cancers: Cryosurgery is not recommended for invasive skin cancers, melanomas (except for lentigo maligna in situ in select cases), or tumors in high-risk locations.
- Recurrence Rate: The recurrence rate for cryosurgery may be slightly higher than for excisional surgery or Mohs surgery, especially for larger or deeper tumors.
- Side Effects: In addition to pigment changes, cryosurgery can cause temporary pain, swelling, redness, and rarely, nerve damage.
5. Laser Surgery: Precision for Superficial Lesions
Laser surgery utilizes focused beams of light to precisely target and destroy abnormal tissue. Different types of lasers are used in dermatology, each with specific wavelengths and applications. For skin cancer, lasers are primarily used for very superficial lesions and precancerous conditions.
Types of Lasers Used in Skin Cancer Surgery:
- Carbon Dioxide (CO2) Laser: This laser is effective for vaporizing (burning away) superficial skin cancers and precancerous lesions. It can be used in a cutting mode for precise excision or in a vaporization mode to remove thin layers of tissue.
- Pulsed Dye Laser (PDL): PDL is primarily used to treat blood vessels and may be helpful for certain superficial skin cancers or precancerous lesions with prominent blood vessels.
When is Laser Surgery Appropriate?
Laser surgery is mainly used for:
- Precancerous Lesions (Actinic Keratoses): CO2 laser vaporization can be effective for treating widespread actinic keratoses.
- Very Superficial Basal Cell Carcinomas (BCCs) in select cases: Laser surgery may be considered for very small, superficial BCCs that are not in high-risk locations and are well-defined.
- Superficial Squamous Cell Carcinomas (SCCs) in select cases: Similar to BCCs, laser surgery is less common for SCCs but may be used for very superficial, low-risk SCCs in specific situations.
- Lentigo Maligna (Melanoma in situ): CO2 laser may be used in some cases of lentigo maligna.
Advantages of Laser Surgery:
- Precise Tissue Removal: Lasers allow for very precise removal of tissue, minimizing damage to surrounding healthy skin.
- Minimal Bleeding: Laser surgery often results in less bleeding compared to traditional surgical excision.
- Reduced Scarring (potentially): In some cases, laser surgery may lead to less noticeable scarring than other surgical methods, especially for superficial lesions.
- Outpatient Procedure: Laser surgery is typically performed in an outpatient setting.
Recovery and Aftercare after Laser Surgery:
- Wound Care: Similar to other surgical procedures, wound care instructions will be provided. The treated area may be red, swollen, and may ooze or crust over.
- Healing Time: Healing time varies depending on the type of laser and the extent of treatment, but it generally takes several weeks.
- Sun Protection: Strict sun protection is crucial after laser surgery to prevent pigment changes and promote healing.
Limitations and When Laser Surgery is Not Suitable:
- Superficial Lesions Only: Laser surgery is primarily effective for very superficial skin cancers and precancerous lesions. It is not appropriate for invasive or deeper tumors.
- Margin Control: Laser surgery does not offer the same level of margin control as Mohs surgery, as the tissue margins are not routinely examined microscopically during the procedure.
- Recurrence Rate: The recurrence rate for laser surgery may be higher than for excisional surgery or Mohs surgery for certain types of skin cancer.
- Pigment Changes: Laser surgery can sometimes cause pigment changes in the treated skin, resulting in lighter or darker patches.
6. Lymph Node Biopsy/Dissection: Addressing Potential Spread
In cases of melanoma and some high-risk squamous cell carcinomas, there is a risk that the cancer may have spread to nearby lymph nodes. Lymph nodes are small, bean-shaped organs that are part of the immune system and can be a site of cancer metastasis. If there is concern about lymph node involvement, lymph node surgery may be necessary.
Types of Lymph Node Procedures:
- Sentinel Lymph Node Biopsy (SLNB): This is a minimally invasive procedure used to determine if cancer cells have spread to the sentinel lymph node(s), which are the first lymph node(s) to which cancer cells are likely to spread from the primary tumor.
- Procedure: Before surgery, a radioactive tracer and/or blue dye is injected near the skin cancer site. These substances travel to the sentinel lymph node(s). During surgery, the surgeon uses a handheld device to detect the radioactive tracer and/or visually identifies the blue dye to locate and remove the sentinel lymph node(s).
- Pathology: The removed sentinel lymph node(s) are examined under a microscope for cancer cells.
- If Sentinel Node is Negative: If the sentinel lymph node is negative (no cancer cells found), it’s highly likely that the cancer has not spread to other lymph nodes, and no further lymph node surgery is needed.
- If Sentinel Node is Positive: If the sentinel lymph node is positive (cancer cells found), it indicates that the cancer has spread to the regional lymph nodes, and a more extensive lymph node dissection may be recommended.
- Lymph Node Dissection (Lymphadenectomy): If the sentinel lymph node biopsy is positive or if there is clinical evidence of lymph node involvement (e.g., enlarged lymph nodes felt during physical examination), a lymph node dissection may be performed. This involves surgically removing a group of lymph nodes in the region of the primary skin cancer.
- Procedure: Lymph node dissection is a more extensive surgery than sentinel lymph node biopsy. The surgeon removes a defined group of lymph nodes in the affected area.
- Pathology: The removed lymph nodes are examined for cancer cells to determine the extent of lymph node involvement (lymph node staging).
When is Lymph Node Surgery Necessary?
Lymph node surgery is primarily considered for:
- Melanoma: Sentinel lymph node biopsy is often recommended for melanomas of intermediate or high thickness to assess for lymph node metastasis. Lymph node dissection may be performed if the sentinel node is positive or if there is clinical evidence of lymph node involvement.
- High-Risk Squamous Cell Carcinoma (SCC): Lymph node surgery may be considered for SCCs with high-risk features, such as large size, deep invasion, perineural invasion (cancer cells invading nerves), or location in certain areas.
Recovery and Aftercare after Lymph Node Surgery:
- Wound Care: Wound care instructions will be provided for the surgical incision(s).
- Pain Management: Pain medication will be prescribed to manage post-operative pain.
- Drainage Tubes: Drainage tubes may be placed in the surgical site to remove excess fluid and prevent fluid buildup (seroma). These are typically removed within a few days.
- Physical Therapy: Physical therapy may be recommended, especially after lymph node dissection, to help restore range of motion and prevent lymphedema (swelling due to lymphatic fluid buildup).
- Lymphedema Risk: Lymph node surgery, particularly lymph node dissection, carries a risk of lymphedema, a chronic swelling condition that can occur in the arm or leg on the side of the surgery. Early detection and management of lymphedema are important.
Importance of Lymph Node Staging:
Lymph node staging is crucial in skin cancer, particularly melanoma and high-risk SCC, as it provides important prognostic information and helps guide further treatment decisions. If lymph node metastasis is present, adjuvant therapies like radiation therapy, chemotherapy, targeted therapy, or immunotherapy may be recommended after surgery to reduce the risk of recurrence and improve survival.
Choosing the Right Surgical Option: A Personalized Approach
Selecting the most appropriate surgical option for skin cancer is a collaborative decision between you and your dermatologist or surgical oncologist. Several factors are carefully considered:
- Type of Skin Cancer: BCC, SCC, melanoma, or other less common types each have different characteristics and treatment approaches.
- Size and Depth of Tumor: Smaller, superficial tumors may be suitable for simpler procedures like C&E or cryosurgery, while larger or deeper tumors may require excision or Mohs surgery.
- Location of Tumor: Tumors in cosmetically sensitive areas (face, neck, hands, feet) often benefit from tissue-sparing techniques like Mohs surgery. Tumors in less visible areas may be treated with excisional surgery or C&E.
- Stage of Cancer: If there is concern about lymph node involvement or metastasis, lymph node surgery may be necessary.
- Patient Health and Preferences: Your overall health, medical history, and personal preferences regarding treatment options are also important considerations.
Consultation with a Specialist:
It’s essential to consult with a board-certified dermatologist or a surgical oncologist specializing in skin cancer to discuss your individual case and determine the best surgical approach for you. During your consultation, be sure to:
- Ask Questions: Don’t hesitate to ask any questions you have about your diagnosis, treatment options, risks, benefits, and expected outcomes.
- Discuss Your Concerns: Share any concerns you have about scarring, pain, recovery, or other aspects of surgery.
- Understand the Procedure: Ensure you fully understand the surgical procedure recommended for you, including what to expect before, during, and after surgery.
- Inquire about Alternatives: Discuss non-surgical treatment options if you are not a candidate for or prefer to avoid surgery.
Personalized Treatment Plans:
Skin cancer treatment is not one-size-fits-all. Your treatment plan should be tailored to your specific situation, taking into account all the factors mentioned above. Your dermatologist or surgical oncologist will work with you to develop a personalized plan that maximizes your chances of cure and achieves the best possible outcome.
Preparing for Skin Cancer Surgery: What You Need to Know
Proper preparation for skin cancer surgery can help ensure a smooth procedure and recovery. Your surgeon will provide you with specific pre-operative instructions, which may include:
- Medical History Review: Inform your surgeon about your complete medical history, including any medical conditions, allergies, and medications you are taking (prescription, over-the-counter, and supplements).
- Medication Adjustments: Your surgeon may advise you to stop taking certain medications, such as blood thinners (aspirin, warfarin, etc.), nonsteroidal anti-inflammatory drugs (NSAIDs like ibuprofen, naproxen), and vitamin E, for a period before surgery, as these can increase the risk of bleeding.
- Lifestyle Adjustments:
- Smoking Cessation: If you smoke, quitting smoking before surgery is highly recommended, as smoking can impair wound healing and increase the risk of complications.
- Alcohol Avoidance: Avoid alcohol consumption for at least 24 hours before surgery, as alcohol can also increase bleeding risk.
- Day of Surgery Instructions:
- Fasting: You may be asked to fast for a certain period before surgery, especially if general anesthesia or sedation is planned.
- Clothing: Wear comfortable, loose-fitting clothing on the day of surgery.
- Transportation: Arrange for someone to drive you home after surgery, especially if you are having sedation or general anesthesia.
- Anesthesia Options: Discuss anesthesia options with your surgeon. Local anesthesia is most common for skin cancer surgery. In some cases, sedation or general anesthesia may be considered, depending on the procedure and patient factors.
- What to Expect on Surgery Day: Your surgeon’s office will provide details about check-in procedures, surgery duration, and what to expect during and immediately after the procedure.
Recovery and Aftercare: Promoting Healing and Minimizing Scarring
Proper post-operative care is crucial for optimal healing, minimizing scarring, and preventing complications after skin cancer surgery. Your surgeon will provide detailed aftercare instructions, which typically include:
- Wound Care:
- Keep the Wound Clean and Dry: Follow your surgeon’s instructions for cleaning the wound, typically involving gentle washing with mild soap and water or saline solution.
- Apply Ointment: Apply a topical antibiotic ointment or petroleum jelly as directed to keep the wound moist and prevent infection.
- Dressing Changes: Change dressings as instructed, usually once or twice daily.
- Pain Management:
- Over-the-Counter Pain Relievers: Mild to moderate pain is common after surgery and can usually be managed with over-the-counter pain relievers like acetaminophen (Tylenol) or ibuprofen (Advil, Motrin).
- Prescription Pain Medication: For more significant pain, your surgeon may prescribe stronger pain medication.
- Signs of Infection: Be vigilant for signs of infection, such as:
- Increased Pain or Tenderness
- Redness, Swelling, or Warmth around the Wound
- Pus or Drainage from the Wound
- Fever or Chills
- If you notice any of these signs, contact your surgeon’s office immediately.
- Scar Management:
- Sun Protection: Strict sun protection is essential for scar healing. Keep the scar covered and apply broad-spectrum sunscreen with an SPF of 30 or higher to the scar area once it has fully healed. Sun exposure can worsen scarring and cause hyperpigmentation (darkening of the scar).
- Scar Massage: Once the wound is fully closed and sutures are removed, gentle scar massage with a moisturizer or silicone-based scar gel can help improve scar appearance over time.
- Silicone Sheeting or Gel: Silicone sheeting or gel can be applied to the scar to help flatten and soften it.
- Laser Treatments or Other Scar Revision Procedures: If scarring is significant or bothersome, your dermatologist may recommend laser treatments or other scar revision procedures to improve its appearance.
- Follow-up Appointments: Attend all scheduled follow-up appointments with your surgeon. These appointments are crucial for:
- Wound Check: To ensure proper healing and monitor for infection.
- Suture Removal: If sutures were used, they will be removed at a follow-up appointment.
- Recurrence Monitoring: To monitor for any signs of skin cancer recurrence at the surgical site or elsewhere.
- Routine Skin Exams: Regular skin self-exams and professional skin exams by your dermatologist are essential for early detection of new skin cancers or recurrences.
Conclusion: Surgery as a Powerful Tool in Skin Cancer Treatment
Surgery is a highly effective and often curative treatment for skin cancer. Understanding the different surgical options available empowers you to be an active participant in your care and make informed decisions in consultation with your dermatologist or surgical oncologist.
Remember, early detection is key to successful skin cancer treatment. Regular skin self-exams and annual professional skin exams can help identify skin cancers in their early stages when surgical treatment is most likely to be curative. If you notice any new or changing moles, spots, or growths on your skin, don’t hesitate to seek medical attention promptly.
With advancements in surgical techniques and a personalized approach to treatment, skin cancer surgery offers hope and excellent outcomes for millions of individuals affected by this common disease. Embrace sun-safe habits, be proactive about skin checks, and know that effective treatment options are available to protect your skin health.
Discover the expertise of Dr. Ebru Okyay, your trusted dermatologist in Antalya. Whether you’re looking to address medical skin concerns or enhance your natural beauty with cosmetic treatments, Dr. Okyay is here to help. With personalized care and advanced techniques, achieving your skin goals has never been easier.
