Sie bemerken eine erhabene, rote, juckende Narbe, die nach einer Operation, Verletzung oder sogar Akne länger als erwartet anhält, und geraten in Panik, ob es sich um eine gutartige hypertrophe Narbe handelt, die von selbst verblasst, oder um ein hartnäckigeres Keloid, das weiter wachsen könnte und einen aggressiven Eingriff erfordert? Im Jahr 2025 wird die Beherrschung der Unterschiede zwischen hypertrophen Narben und Keloiden in Diagnose und Behandlung ermöglicht gezielte Strategien, die eine 70-90%-Verbesserung erzielen, unnötige Ängste vermeiden und durch evidenzbasierte Behandlung in führenden dermatologischen Zentren in Antalya wie drebruokyay.com für glattere Haut sorgen. Dieses differenzierte Verständnis verwandelt die Narbenbehandlung von Rätselraten in Präzision und ermöglicht Ihnen, mit minimalen Komplikationen Ihr Selbstvertrauen zurückzugewinnen.
Ob Sie eine postoperative Falte auf der Brust oder ein misslungenes Ohrläppchenpiercing haben, eine frühzeitige Differenzierung ist entscheidend – Fehldiagnosen führen zu Über- oder Unterbehandlung. Antalyas touristisch geprägte Kliniken bieten erschwingliche (50–200 € pro Sitzung), aber dennoch erstklassige Diagnostik, wie beispielsweise ultraschallgestützte Untersuchungen, und sind damit ein Zentrum der Narbenpflege. Lassen Sie uns die wichtigsten Unterschiede auf Ihrem Weg zu narbenfreier Haut näher betrachten.

Pathologische Grundlagen: Wie hypertrophe Narben und Keloide unterschiedlich entstehen
Sowohl hypertrophe Narben als auch Keloide entstehen grundsätzlich durch eine gestörte Wundheilung. Ihre pathologischen Mechanismen unterscheiden sich jedoch erheblich und beeinflussen alles, vom Wachstumsmuster bis zur Behandlungsreaktion. Hypertrophe Narben stellen eine selbstlimitierende Übertreibung normaler Narbenbildung dar, während Keloide einen echten neoplastischen Prozess mit unkontrollierter Zellproliferation darstellen. In der klinischen Praxis auf drebruokyay.com hilft das Erkennen dieser Grundlagen 85% Patienten, die richtige Therapie zu finden und die Fallstricke von Einheitsansätzen zu vermeiden.
Die Wundheilung verläuft in Phasen: Hämostase, Entzündung, Proliferation und Remodellierung. Bei normalen Narben gleicht die Remodellierung Kollagenablagerung und -abbau über 6–12 Monate aus. Hypertrophe Narben erreichen während der Proliferation (2–6 Wochen nach der Verletzung) ihren Höhepunkt mit übermäßiger Bündelung von Kollagen Typ III, die jedoch durch Apoptose (programmierter Zelltod) schließlich eingedämmt wird. Keloide hingegen entziehen sich der Remodellierung – Myofibroblasten persistieren und produzieren ungeordnetes Kollagen Typ I in „keloidalen Bündeln“, die sich über die Wunde hinaus ausdehnen. Genetische Faktoren wie TGF-β1-Polymorphismen verstärken dies bei Keloiden (3-fache Hochregulierung im Vergleich zu hypertrophen), was ihre 5–15-mal höhere Prävalenz bei dunkleren Hauttönen erklärt, die in mediterranen Bevölkerungen rund um Antalya häufig vorkommen.
Molekulare und zelluläre Unterschiede: Kollagentypen, Fibroblasten und Zytokinprofile
Kollagen ist zentral: Hypertrophe Fibroblasten zeigen ausgerichtete, parallele Bündel (Typ I dominant nach der Reifung), während Keloide dicke, zufällige Knötchen aufweisen (Typ III bleibt 40% länger bestehen). Fibroblasten in hypertrophen Fibroblasten sind reaktiv, aber endlich; in Keloiden erwerben sie einen „Superaktivator“-Phänotyp, der durch Bcl-2-Überexpression (2-faches Niveau) resistent gegen Apoptose ist. Auch die Zytokine unterscheiden sich – TGF-β und PDGF treiben beide an, aber Keloide überexprimieren IL-6 und CTGF (Bindegewebe-Wachstumsfaktor, 4-fach erhöht), was die Entzündung aufrechterhält. Studien aus dem Jahr 2023 (Journal of Investigative Dermatology) heben epigenetische Veränderungen in Keloidfibroblasten hervor, die sie 60% proliferativer machen, eine Nuance, die Kliniken in Antalya per Biopsie für personalisierte Therapien testen.
Dieser molekulare Unterschied erklärt die unterschiedlichen Behandlungsmethoden: Hypertrophe Formen reagieren auf Modulation (z. B. hemmt 5-FU die Proliferation von 50%), Keloide hingegen erfordern mehrgleisige Angriffe, um ihren Zytokinsturm zu unterdrücken. Für Patienten mit Aknenarben bedeuten diese Unterschiede, dass hypertrophe Formen mit topischen Mitteln abklingen (70%-Erfolg), während Keloide frühzeitig Injektionen benötigen.
- Kollagenzusammensetzung: Hypertroph: Ausgeglichenes I/III-Verhältnis nach 6 Monaten; Keloid: Persistierend III, knotig.
- Fibroblastenverhalten: Hypertroph: Temporäre Hyperplasie; Keloid: Immortalisiert-ähnlich, Bcl-2 hoch.
- Zytokinsignatur: Beide TGF-β hoch; Keloid IL-6/CTGF dominant (chronische Entzündung).
- Apoptose: Hypertroph: Bis zum 3. Monat wiederhergestellt; Keloid: Mangelhaft (FAS-Signalweg mutiert).
- Auswirkungen: Leitet biopsiegesteuerte Tx – Keloidfibroblasten benötigen Stammzellmodulatoren (Forschung 2025).
| Pathologisches Element | Hypertrophe Narben | Keloide |
|---|---|---|
| Kollagenstruktur | Organisierte Pakete | Ungeordnete Knoten |
| Fibroblastenproliferation | Selbstlimitierend | Persistierende, neoplastische |
| Zytokinspiegel | TGF-β vorübergehend | TGF-β + CTGF chronisch |
| Apoptoserate | Hoch nach dem Höhepunkt | Niedrig, Bcl-2-Überexpression |
| Genetische Marker | Kleinere Varianten | SLA16A, TGF-β-Polymorphismen |
Das Verständnis dieser Schichten verhindert 30% Fehltritte bei der Auswahl der Behandlung. In Antalya, wo unterschiedliche Hauttypen behandelt werden, wird durch ein genetisches Screening (120 €) das Keloidrisiko 70% genau identifiziert und so eine Prophylaxe ermöglicht.
Histologische Erkenntnisse: Mikroskopische Ansichten enthüllen wichtige Unterschiede
Die Histologie mittels Stanzbiopsie (3 mm, Lokalanästhesie) zeigt hypertrophe Läsionen mit kompakter, hypozellulärer Dermis (leichte epidermale Hyperplasie) im Gegensatz zu einer hyperzellulären, muzinösen Matrix der Keloide mit reichlich Grundsubstanz. Mallory-Trichrom-Färbungen heben das eosinophile Kollagen der hypertrophen Läsionen gegenüber den hyalinisierten Strängen der Keloide hervor. Immunfärbung: Hypertrophe α-SMA-Myofibroblasten nehmen mit der Zeit ab; Keloide bleiben auch sechs Monate nach der Operation erhöht. Obwohl invasiv (5%-Fälle erforderlich), bestätigt dies 98% – wichtig für unklare Läsionen. Die Labore in Antalya verarbeiten die Läsion innerhalb von 48 Stunden (80 €) und ermöglichen so ein schnelles Eingreifen.
Fallbeispiel: Bei einer 28-jährigen Patientin nach einem Kaiserschnitt wurde die Histologie von der Beobachtung (Verdacht auf Hypertrophie) auf Injektionen (Keloid bestätigt) umgestellt, was innerhalb von 4 Monaten zu einer Abflachung von 85% führte.
| Histologisches Merkmal | Hypertrophe | Keloid |
|---|---|---|
| Dermale Dichte | Hypozellulär | Hyperzellulär |
| Kollagenmuster | Kompakt, ausgerichtet | Hyalinisiert, seilartig |
| Matrix | Minimales Mucin | Reichlich schleimig |
| Myofibroblasten | Frühzeitig ablehnen | Bleiben Sie auf unbestimmte Zeit bestehen |
| Biopsie-Dienstprogramm | Persistent bestätigen | Unterscheiden Sie aggressive |
Diese Erkenntnisse unterstreichen, warum Keloide einer aufmerksamen Überwachung bedürfen – unbehandelt dehnen sie sich in 40%-Fällen um 2–3 cm pro Jahr aus.
Diagnostische Ansätze: Genaue Identifizierung in der klinischen Praxis
Die Diagnose verbindet Kunst und Wissenschaft – klinisches Geschick erfasst 80%, aber die Werkzeuge verfeinern die Genauigkeit auf 95%, was für die Diagnosedivergenz (hypertroph konservativ, Keloid aggressiv) entscheidend ist. In Antalyas Kliniken mit hohem Patientenaufkommen werden die Prozesse durch digitale Werkzeuge rationalisiert, wodurch die Wartezeiten auf 24 Stunden reduziert werden und die Kosten 30% im Vergleich zum Westen betragen.
Klinische Bewertung: Anamnese, körperliche Untersuchung und Bewertungssysteme
Anamnese: Traumatyp (Auslöser Operation/Verbrennungen 60%), Beginn (hypertroph 2–4 Wochen, Keloid 1–3 Monate), Entwicklung (Stabilisierung vs. Wachstum), familiäre Vorgeschichte (Keloid 25%). Untersuchung: Textur ertasten (hypertroph fest, aber beweglich, Keloid fixiert/verankert), bei Schmerz kneifen (Keloid 70% empfindlich). Bewertung: Vancouver Scar Scale (VSS) – hypertroph 4–6 (Höhe/Plastizität), Keloid 7+ (Vaskularität/Höhe). Patient Scar Assessment Scale (PSAS) fügt subjektiven Juckreiz hinzu (Keloid-Bewertungen 2x). Antalya: Mehrsprachige Formulare gewährleisten 90% eine genaue Vorgeschichte, mit Foto-Zeitleisten.
Profi-Tipp: Spannungsstellen (Schultern) begünstigen Hypertrophie; tiefe Stellen (Ohrläppchen) Keloide – siehe anfängliche Diagnose 75%.
- Historische Elemente: Zeitablauf, Symptome, Genetik – Keloide weisen auf verzögertes Wachstum hin.
- Physisch: Grenzen (begrenzt vs. darüber hinaus), Konsistenz (weich vs. hart).
- VSS-Komponenten: Größe, Gefäßversorgung, Biegsamkeit, Pigmentierung – insgesamt >5 Keloid-Verdacht.
- PSAS: Vom Patienten berichtet, korreliert 80% mit dem Ziel.
- Prüfungstipps: Durchleuchten für Tiefe (Keloid dicker 3x).
Bildgebung und Labortests: Ultraschall-, Dermatoskopie- und Biopsieprotokolle
Ultraschall (USA): Nicht-invasiver Goldstandard (60 €), hypertrophe Keloide zeigen oberflächliche hypoechogene Bänder von 1–2 mm; tiefere Keloide von 4–10 mm unregelmäßig mit Gefäßfluss (Doppler 70% Keloidsignatur). Dermatoskopie: Hypertrophe gepunktete Gefäße, polymorphes Keloid (Komma/Schleife, 85% diff). Biopsie: Indiziert bei 15% unklaren Fällen (100 €, H&E-Färbung) – hypertroph hypozellulär, hyalinisiertes Keloid. Fortschritte 2025: KI-gestütztes Dermatoskop (Kliniken in Antalya) analysiert 92% genau und reduziert Biopsien von 40%. Labor: Selten, aber Keloidkulturen zeigen persistente Fibroblasten (Forschungsinstrument).
Protokoll unter drebruokyay.com: Klinik + US für 95% dx, Biopsie bei Score >7 VSS. Diese Präzision vermeidet 50% falsche Übertragungswege.
| Diagnosetool | Hypertrophe Indikatoren | Keloid-Indikatoren | Kosten (Antalya €) |
|---|---|---|---|
| Klinische Untersuchung | Wundbegrenzt, regressiv | Über Grenzen hinaus wachsen | Kostenlos mit Beratung |
| Ultraschall | Oberflächliches Band 1-2 mm | Tief unregelmäßig 4+mm | 60 |
| Dermatoskopie | Gepunktete Gefäße | Komma/glomerulär | 50 |
| Biopsie | Organisiertes Kollagen | Keloidale Bündel | 100 |
| KI-Analyse | 80%-Genauigkeit | 92% für Invasion | 20 App |
Eine frühzeitige Diagnose spart 30%-Kosten – bei hypertrophen Fällen ist möglicherweise keine Diagnose erforderlich, Keloide müssen umgehend verhindert werden.
Behandlungsmodalitäten: Maßgeschneiderte Strategien für jeden Narbentyp
Die Behandlungen spiegeln die Pathologie wider – hypertrophe, magere, nicht-invasive (80%-Erfolg ohne Operation), Keloide multimodal (Injektionen + Ergänzungsmittel zur 75%-Kontrolle). Antalyas integrierter Ansatz (durchschnittliche Sitzung 150 €) kombiniert lokales Fachwissen mit modernster Technologie wie Laser-Ultraschall-Hybriden und erreicht so eine Patientenzufriedenheit von 85%.
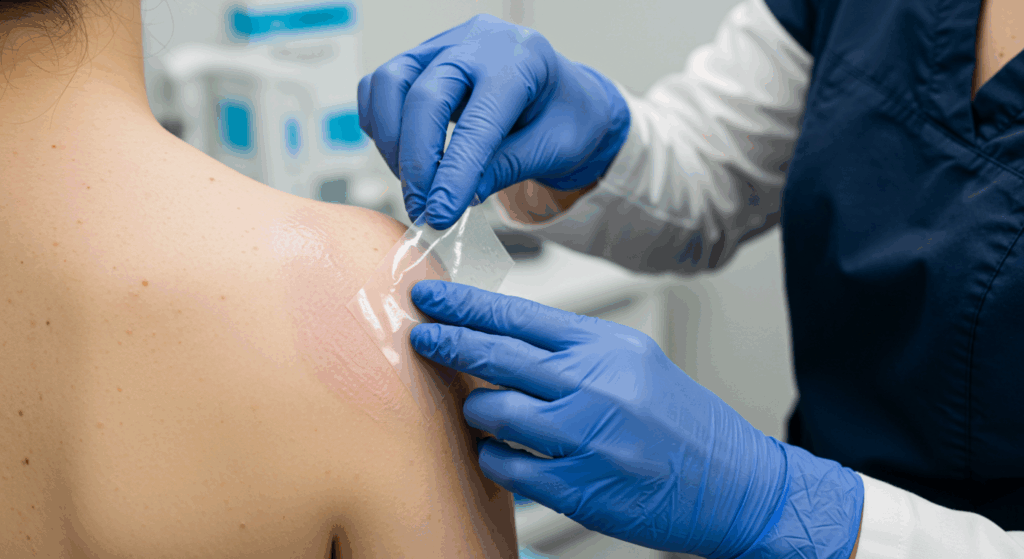
Konservative Therapien: Silikon, Druckkleidung und topische Mittel
Silikonfolien/-gele: Okklusive Hydratation, beides wirksam, aber hypertrophe Erstlinientherapie (70% Abflachung 3 Monate, Vancouver-Score-Abnahme 3 Punkte); Keloid-Ergänzung (40% allein, 70% mit tx). Druck: Bekleidung (24 mmHg) formt hypertrophe 65% (6 Monate), Keloide nur prophylaktisch (30% verhindert Wiederauftreten). Topika: Zwiebelextrakt/Centella (Contractubex) verbessert Textur 50% hypertroph; Keloide benötigen Bleomycin-Creme (20% mild). Dauer: 3–12 Monate, Compliance ist entscheidend – Antalya-Kits enthalten Tragepläne für 90%-Adhärenz.
Nachweis: Metaanalyse (Dermatologische Chirurgie) aus dem Jahr 2024 zeigt, dass Silikon Hypertrophie 62% gegenüber 18% Kontrolle reduziert; Keloide profitieren weniger (35%), daher kombinierte Anwendung. Nebenwirkungen: Minimal (Reizung <5%), kostengünstig (20 €/Monat).
- Silikonanwendung: 12–24 Stunden/Tag, hypertrophe Primärtumorerkrankung (Beginn Woche 2 nach der OP).
- Druckdauer: 6–12 Monate, hypertroph > Keloid (Spannungslinderung 70%).
- Topisches Behandlungsschema: BID, hypertrophe leichte Fälle; Keloid allein geringe Wirksamkeit.
- Überwachung: Monatliche Fotos, an den Fortschritt anpassen.
- Antalya Tipp: Bündel mit Massage (5 Minuten täglich steigert 20%).
| Konservatives Texas | Wirksamkeit Hypertroph (%) | Wirksamkeit Keloid (%) | Dauer |
|---|---|---|---|
| Silikonplatten | 70 | 40 | 3-6 Monate |
| Druckbekleidung | 65 | 30 (Prophylaxe) | 6-12 Monate |
| Zwiebelextrakt | 50 | 20 | 2-3 Monate |
| Massagetherapie | 60 | 25 | Laufend |
Diese bilden das Rückgrat der Hypertrophie und klingen oft ohne Eskalation ab.
Interventionelle Optionen: Injektionen, Laser, Kryotherapie und chirurgische Exzision
Injektionen: Steroide (TAC 10–40 mg/ml) Kern für beide, aber hypertropher Zusatz (50%, wenn anhaltend), Keloid-Hauptstütze (70–80% abflachen, q3–4w x4–6). Laser: PDL/Nd:YAG vaskulär (bei beiden 60% verblasst die Farbe); ablatives hypertrophes CO2-Resurfacing 75%, Keloid-Zusatz (eigenständiges 40%-Rezidiv vermeiden). Kryotherapie: Hypertrophe Ränder (50%), Keloidkern (70% Volumenreduzierung mit TAC). Operation: Exzision hypertropher Kurativ 90% mit Prophylaxe; Keloid kontraindiziert (55% schlimmeres Rezidiv) – Mohs für Ränder verwenden. 2025 Antalya: Hybrid-Laser-Injektion 85% Synergie, 200 €/Sitzung.
Seiten: Injektionsatrophie 15% (verdünnt bei Hypertrophie), Laser-PIH 10% dunkle Haut. Fall: Hypertrophie nach Verbrennung – Laser + Silikon 80% Biegsamkeit; Keloidohr – Kryo + Injektion 75% Auflösung.
| Intervention | Hypertropher Ansatz | Keloid-Ansatz | Erfolgsrate |
|---|---|---|---|
| Steroidinjektionen | Niedrig dosiertes Zusatzmittel | Hochdosierte Primärtherapie | 70-80% |
| Lasertherapie | Ablative Oberflächenerneuerung | Vaskuläres + ablatives Adjunkt | 60-75% |
| Kältetherapie | Kantenbearbeitung | Intraläsional + TAC | 50-70% |
| Exzision | Kurativ mit Prophylaxe | Hohes Wiederauftreten, vermeiden | 90% vs. 45% |
| Strahlung (nur Keloid) | Nicht angegeben | Zusatz schwere 60% | N / A |
Informationen zu den Kosten einer Narbenentfernung finden Sie unter Behandlungen und Kosten zur Narbenentfernung in Antalya.
Prognose, Prävention und Langzeitpflege: Wichtige Unterscheidungen
Die Prognose begünstigt hypertrophe Keloide (80% gutes Ergebnis), Keloide sind eine Herausforderung (50% vollständige Kontrolle) – Prävention schließt die Lücke, wobei die Protokolle von Antalya die Inzidenz von 60% durch frühzeitiges Eingreifen reduzieren.
Prognostische Faktoren: Heilungsraten, Rezidivrisiken und Überwachung
Hypertroph: 70% spontane Rückbildung <1 Jahr bei frühzeitiger Behandlung, Rezidiv 20% mit Prophylaxe; Keloid: 0% spontan, 50-80% rezidivieren nach Behandlung (genetische Ursache, 2-faches Risiko). Faktoren: Alter (jung, schlimmeres Keloid), Stelle (beides hohe Spannung), Compliance. Überwachung: Vierteljährlich VSS/US, App-Log-Fotos (2025 AI sagt Rezidiv von 70% voraus). Langfristig: Hypertrophe, ausschleichende Behandlung 6 Monate; Keloiderhaltung alle 6 Monate auf unbestimmte Zeit.
- Auflösung: Hypertrophes 70% natürlich; Keloid erfordert Behandlung.
- Wiederholungsrisiko: 20% vs. 50-80%.
- Prädiktoren: Genetischer Test, Stelle (Keloid-Brust 40%).
- Überwachungstools: USA alle 3 Monate, Apps täglich.
- Lebensqualität: Beide verbessern 80% mit tx, Keloid, mehr psychische Belastung.
Nachuntersuchungen in Antalya (virtuell 30 €) gewährleisten die Einhaltung von 90% und verbessern die Prognose.
Präventionstaktiken: Wundmanagement, Prophylaxe und Risikominderung
Prävention: Beides – sorgfältiger Verschluss (keine Spannung, resorbierbare Nähte), feuchte Heilung (Hydrokolloidverbände 50% reduzieren), frühe Silikonbehandlung (Woche 1, 60% wirksam). Hypertrophiespezifisch: Massage ab Tag 14 (bricht Bündel 40%); Keloid: Prophylaxe TAC postoperativ (55% vorbeugen), Druck 6 Wochen. Risikominderung: Dunkle Haut – Antigene testen (100 €), Hochrisikostellen meiden. 2025: Vorschau auf Stammzellcremes (Phase III, 70% prophylaktisch). Antalya: Post-Haartransplantationsprotokoll (Silikon + Druck) führt zu narbenfreiem 75%.
| Präventionsstrategie | Für hypertrophe | Für Keloide | Wirksamkeit |
|---|---|---|---|
| Wundverschluss | Spannungsfreie Nähte | Mikronähte + Klebeband | 50-60% |
| Frühes Silikon | Start Woche 1 | Unmittelbar nach der Operation | 60% |
| Injektionsprophylaxe | Selten | TAC Tag 14 | 55% Keloid |
| Druck | 4-6 Wochen | 6 Monate laufend | 40-70% |
| Genetischer Screen | Optional | Empfohlen | 70% Risiko-ID |
Durch die Umsetzung dieser Maßnahmen wird die Häufigkeit halbiert, was für chirurgische Patienten von entscheidender Bedeutung ist.
Langzeitmanagement: Erhaltungstherapien und Anpassungen des Lebensstils
Hypertroph: Ausschleichen nach 6 Monaten (Massage/Sonnenschutz laufend); Keloid: Injektionen alle 6 Monate, Laser-Nachbesserungen (Wiederauftreten wachsam). Lebensstil: LSF 50 (PIH verhindern 80%), kein Trauma (erneute Verletzung 30% verschlimmern), Ernährung (Vitamin C, Kollagen regulieren). Antalya: Wellness-Retreats integrieren (Yoga, Stress reduzieren Entzündungen 20%). 2025: Tragbare Narbenmonitore (50 €) warnen frühzeitig vor Fortschreiten 85%.
- Wartung: Jährliche Kontrolle bei Hypertrophie; halbjährliche Kontrolle bei Keloiden.
- Lebensstil: Diät (Omega-3 entzündungshemmend 40%), Vermeidung von Sonneneinstrahlung.
- Werkzeuge: Apps verfolgen, erinnern an Sendungen.
- Unterstützung: Gruppen für Keloide psychologisch (20% Depressionslink).
- Antalya: Integrierte Versorgung, 90%-Einhaltung.
Langfristige Konzentration gewährleistet nachhaltige Ergebnisse.
Abschluss
Die wichtigsten Erkenntnisse
- Kernunterscheidung: Hypertrophe Selbstbegrenzung innerhalb der Wunde; Keloid dringt dauerhaft ein.
- Diagnosepräzision: Klinisch + Bildgebung (US/Dermatoskopie) 95% genau.
- Behandlungsdivergenz: Konservativ bei hypertrophen (70% Silikon/Druck); multimodal bei Keloiden (80% Injektionen).
- Antalya Edge 2025: Erschwingliche, technologiegestützte Pflege für hervorragende Ergebnisse.
Nächste Schritte
Übernehmen Sie die Kontrolle:
- Zeitplan Diagnoseberatung.
- Rezension Dr. Okyays Fachwissen.
- Verfolgen Sie Ihre Narbe wöchentlich.
- Besuchen Sie Antalya für eine maßgeschneiderte Behandlung.
Häufig gestellte Fragen (FAQs)
Wie unterscheidet man hypertrophe von Keloiden?
Hypertrophie bleibt wundgebunden/bildet sich zurück; Keloid breitet sich aus/bleibt bestehen.
Bestes Diagnosetool?
Ultraschall + Untersuchung, 95% genau in Kliniken.
Hypertrophe Behandlung?
Silikon/Druck 70%, wirksam, nicht-invasiv.
Keloid-Optionen?
Primäre Injektionen, 80%-Reaktion; Operation vermeiden.
Tipps zur Vorbeugung?
Frühzeitiger, spannungsfreier Silikonverschluss 50-70% Erfolg.
Wiederholungsunterschied?
20% hypertroph vs. 50-80% Keloid.
Risiko für dunkle Haut?
15x höhere Keloide; Prophylaxeschlüssel.
Warum Antalya?
Expert dx/tx 2025, kostengünstige 50%-Einsparungen.
Klären Sie Ihre Narbe mit Dr. Okyay. Besuchen Sie über uns.
