Discovering a new lump or bump on the skin can be a cause for concern. While most skin lumps are benign (non-cancerous) and pose no threat to health, some can be signs of inflammatory conditions requiring medical management or, in rare cases, indicate a more serious issue like skin cancer. Among the most common types of skin lumps encountered are nodules and cysts.
Understanding what these terms mean, their potential causes, and how they are properly diagnosed and treated is crucial. For individuals in or considering seeking treatment in Turkey, exploring Nodules and Cysts Treatment in Antalya offers access to qualified dermatologists and healthcare facilities equipped to provide expert evaluation and care for these common skin lesions. From a dermatologist’s perspective, the key to managing nodules and cysts effectively is accurate diagnosis – determining exactly what the lump is – to ensure the most appropriate and safe treatment plan is implemented.
The skin is a dynamic organ, and various structures within it and the underlying tissue can give rise to palpable (able to be felt) lumps. While patients may use broad terms like “lump,” “bump,” or “growth,” medical professionals classify these lesions more specifically based on their characteristics, location, and the type of tissue involved. Nodules and cysts represent distinct categories of skin lesions that require different diagnostic considerations and often different treatment approaches.
While many are simple benign findings, neglecting professional evaluation of any new or changing skin lump is not advisable due to the importance of ruling out malignancy (cancer). In a city like Antalya, with its developed healthcare infrastructure, individuals have access to the necessary expertise for the proper diagnosis and management of these common dermatological concerns.

Defining Nodules and Cysts: Understanding the Terms
In dermatology, precise terminology is used to describe skin lesions. While both nodules and cysts are types of “lumps” or “bumps,” they have distinct characteristics.
- Nodule: A nodule is a solid, raised lump within the skin (dermis) or extending deeper into the underlying subcutaneous tissue. By definition, it is usually larger than 1 centimeter (about half an inch) in diameter. Nodules can arise from various tissues within the skin, including an overgrowth of skin cells, fat cells, inflammatory cells, or other abnormal cellular proliferation. They feel firm or hard to the touch. Examples include benign growths like lipomas (fatty tumors), inflammatory lesions like deep acne nodules or those seen in hidradenitis suppurativa, or unfortunately, sometimes malignant lesions like certain skin cancers or metastases to the skin.
- Simple Explanation: A solid lump in or under the skin that’s usually bigger than a pea.
- Cyst: A cyst is a sac-like structure within the skin (dermis) or subcutaneous tissue that contains fluid or semi-solid material. A true cyst has a lining (a layer of cells, often epithelial cells) that produces the contents within the sac. Cysts feel somewhat firm but can also feel slightly softer or even fluctuant (like they contain liquid) depending on the contents and their location. Common examples include epidermoid cysts (often miscalled “sebaceous cysts”) or pilar cysts.
- Simple Explanation: A lump under the skin that’s like a small bag or sac filled with liquid or thick material.
Key Difference: The fundamental difference between a nodule and a cyst is the presence of a sac-like structure containing material in a cyst, versus a solid mass of tissue in a nodule. This distinction is important for understanding how they form and how they are treated (removing the entire sac is key for preventing cyst recurrence).
These definitions are based on clinical appearance and feel, but a definitive classification and diagnosis often require microscopic examination of the tissue (histopathology) after a biopsy or surgical removal.

The Importance of Proper Diagnosis: Don’t Guess, Get it Checked
While many nodules and cysts turn out to be benign and harmless, it is critical to have any new or changing lump on your skin evaluated by a medical professional, ideally a dermatologist. Self-diagnosis or assuming a lump is “just a cyst” is risky because several conditions, including skin cancers, can initially appear as skin nodules or lumps.
- Wide Range of Causes: Skin lumps can be caused by dozens of different conditions, ranging from very common benign growths (like epidermoid cysts, lipomas) and self-limiting inflammatory reactions (like a resolving boil) to chronic inflammatory diseases (like severe acne, hidradenitis suppurativa) and malignant tumors (like basal cell carcinoma, squamous cell carcinoma, melanoma, or metastases to the skin).
- Risk of Misidentification: Relying solely on visual appearance or feel can lead to misidentifying a potentially harmful lesion as something benign. A skin cancer that is growing or changing needs timely diagnosis and treatment to prevent it from spreading and becoming more difficult to treat.
- Appropriate Treatment: Even among benign lesions, the appropriate treatment depends on the specific type. For example, treating an infected cyst requires drainage, while a lipoma usually requires surgical excision for removal. Treating an inflammatory nodule often involves medical therapy rather than just removal. Using the wrong approach can be ineffective, cause complications, or lead to scarring.
Therefore, the first and most important step when you notice a nodule or cyst on your skin is to seek professional medical evaluation. A dermatologist has the specialized knowledge and experience to assess the lesion, consider the range of possible diagnoses, and determine if further testing or treatment is necessary.
The Dermatologist’s Approach to Diagnosis: Uncovering the Cause
Diagnosing a skin nodule or cyst involves a systematic approach combining patient history, clinical examination, and sometimes specific diagnostic procedures.
- Detailed Patient History: The dermatologist will ask questions to understand the story of the lesion:
- When did you first notice the lump?
- Has it changed in size, shape, color, or symptoms (pain, itching, discharge) over time?
- Did it appear after any specific event (e.g., injury, insect bite)?
- Do you have any associated symptoms (e.g., fever, chills, widespread rash)?
- Have you had similar lumps in the past?
- Do you have a personal or family history of skin cancers or other skin conditions?
- What is your occupation or any hobbies that might involve exposure to irritants or potential injury?
- Clinical Examination: The dermatologist will carefully examine the lesion visually and by touch (palpation):
- Location: Where is the lump located on the body? (Some lesions are more common in specific areas).
- Size and Shape: How large is it? Is it round, oval, or irregular?
- Color: What color is it? (Flesh-colored, red, brown, black, yellowish).
- Consistency: How does it feel when pressed? (Soft, firm, hard, rubbery, fluid-filled/fluctuant).
- Mobility: Does it move freely under the skin, or is it attached to the overlying skin or deeper tissues?
- Tenderness: Is it painful when touched?
- Surface Characteristics: Is the overlying skin smooth, scaly, crusted, or does it have a central opening (punctum)?
- Associated Changes: Is there surrounding redness, swelling, or signs of infection?
- Differential Diagnosis: Based on the history and clinical exam, the dermatologist will form a list of possible diagnoses that could explain the lesion. This list, known as the differential diagnosis, includes various benign, inflammatory, and potentially malignant conditions that can present as a nodule or cyst in that location with those characteristics. For example, a firm lump on the back might be an epidermoid cyst, a lipoma, a dermatofibroma, or potentially a skin cancer metastasis or other less common growth.
- Diagnostic Procedures: Often, based on the clinical assessment, the dermatologist can make a presumptive diagnosis. However, in many cases, particularly if the diagnosis is uncertain, if there are any features suggestive of malignancy, or if the lesion is being removed, a diagnostic procedure is performed.
- Skin Biopsy: This is the most definitive diagnostic tool. It involves removing a small sample of the lesion (or the entire small lesion) for microscopic examination by a dermatopathologist (a doctor specializing in diagnosing skin diseases from tissue samples).
- Purpose: Microscopic examination (Histopathology) allows the pathologist to identify the exact type of cells that make up the lesion, confirm if it is benign or malignant, and provide a definitive diagnosis (e.g., “Epidermoid Cyst,” “Lipoma,” “Basal Cell Carcinoma”).
- Types of Biopsy: The type of biopsy chosen depends on the size and nature of the lesion:
- Shave Biopsy: Removal of the superficial layers of the lesion with a sharp blade. Often used for raised lesions where malignancy is suspected superficially.
- Punch Biopsy: Removal of a cylindrical core of tissue using a circular punch tool. Used for lesions extending into the dermis or subcutaneous tissue, or when a full-thickness sample is needed.
- Excisional Biopsy: Removal of the entire visible lesion with a margin of surrounding normal tissue. Often used for smaller nodules or cysts where complete removal is the intended treatment and also provides tissue for diagnosis. It is the preferred method if malignancy is strongly suspected or cannot be ruled out by other biopsy types.
- Simple Explanation: Taking a small piece of the lump (or the whole small lump) and sending it to a lab to be looked at under a microscope to see exactly what kind of cells it’s made of.
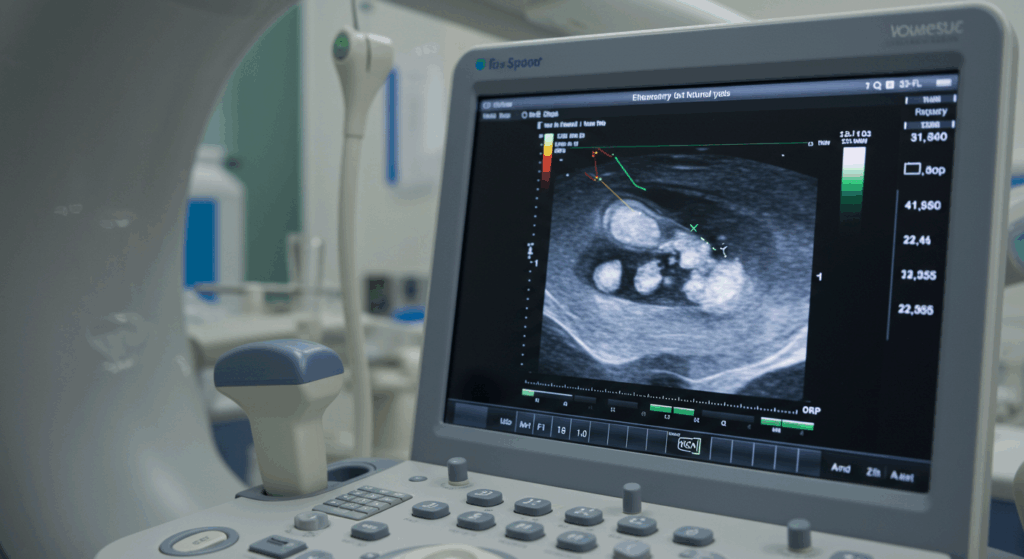
- Imaging: For deeper nodules or lumps where it’s important to see their relationship to underlying structures (muscle, nerves) or confirm their composition (e.g., fatty nature of a lipoma), imaging techniques like ultrasound or MRI may be used.
- Needle Aspiration: Using a fine needle and syringe to draw out fluid or contents from a cyst or suspected abscess. This can be diagnostic (e.g., identifying pus, fluid type) and sometimes therapeutic (reducing swelling). However, it doesn’t provide tissue for histopathology or remove the cyst lining.
- Skin Biopsy: This is the most definitive diagnostic tool. It involves removing a small sample of the lesion (or the entire small lesion) for microscopic examination by a dermatopathologist (a doctor specializing in diagnosing skin diseases from tissue samples).
The information gathered from the history, clinical exam, and any diagnostic procedures allows the dermatologist to establish an accurate diagnosis, which is the essential basis for recommending the most appropriate treatment.
Common Types of Benign Nodules and Cysts: Non-Cancerous Lumps
Many skin nodules and cysts are benign (non-cancerous) and common. While not medically threatening, they can be bothersome due to their size, location, potential for inflammation, or cosmetic appearance.
Epidermoid Cysts (Often Called “Sebaceous Cysts”)
- What they are: These are the most common type of cutaneous (skin) cyst. They arise from the infundibulum (upper part) of a hair follicle. The term “sebaceous cyst” is technically incorrect because these cysts are filled with keratin (skin protein) and sometimes sebum, and are lined by epidermal cells, not cells from the sebaceous gland itself.
- Formation: They form when the opening of a hair follicle gets blocked, often due to trauma, inflammation, or developmental factors. Cells from the follicular wall continue to proliferate inward, forming a sac lined by epidermal cells. These cells produce keratin, which fills the sac over time, sometimes mixing with sebum (oil) from nearby glands.
- Clinical Presentation: Typically present as firm, round, flesh-colored to yellowish lumps just under the skin. They often have a small, dark central opening or pore, called a punctum, which is the blocked opening of the hair follicle. Common locations include the face, neck, trunk, scrotum, and scalp. They can vary in size from a few millimeters to several centimeters.
- Potential Issues: While often asymptomatic, epidermoid cysts can become problematic. They are prone to inflammation (redness, pain, swelling) if the sac wall ruptures under the skin, causing an inflammatory reaction to the keratin contents. They can also become infected with bacteria, leading to an abscess (collection of pus). Sometimes, a cheesy, foul-smelling material can be expressed from the central punctum.
- Diagnosis: Usually diagnosed clinically based on their appearance, feel, and the presence of a central punctum. Definitive confirmation is made by histopathology after removal.
- Management:
- Observation: If the cyst is small, asymptomatic, and the diagnosis is certain, observation is an option.
- Incision and Drainage (I&D): If the cyst is inflamed or infected and has formed an abscess (feels fluctuant, contains pus), incision and drainage is often performed to release the pus and reduce inflammation and pain. Simple Explanation: Making a cut in the lump to let out the pus or build-up. However, I&D does not remove the cyst sac lining, so the cyst is likely to recur once the inflammation subsides.
- Surgical Excision: The preferred treatment for complete removal of the cyst and prevention of recurrence, especially if it is symptomatic, repeatedly inflamed, large, or bothersome for cosmetic reasons. This involves cutting out the entire cyst sac under local anesthetic. Simple Explanation: Cutting out the whole bag-like lump, including its wall, so it doesn’t grow back.
Pilar Cysts (Often Called “Wen”)
- What they are: These are the second most common type of cutaneous cyst. They typically arise from the outer root sheath of a hair follicle. They are less common than epidermoid cysts on most body sites but are the most common type of cyst found on the scalp.
- Formation: Similar to epidermoid cysts, they form a sac, but the lining is composed of cells from a different part of the hair follicle. The sac fills with keratin.
- Clinical Presentation: Present as smooth, firm, mobile, round lumps under the skin. They are almost exclusively found on the scalp. Unlike epidermoid cysts, they usually do not have a central punctum and are less likely to become inflamed or infected, though it can happen. They are often multiple and tend to run in families (autosomal dominant inheritance).
- Diagnosis: Usually diagnosed clinically based on their characteristic appearance and location on the scalp. Histopathology confirms the diagnosis after removal.
- Management: Often observed if asymptomatic. Surgical excision is performed if they are large, bothersome, symptomatic, or for cosmetic reasons. Excision is curative if the entire sac is removed.
Lipomas
- What they are: These are benign tumors composed of mature fat cells (adipocytes). They are very common.
- Formation: They form as an overgrowth of fat cells in the subcutaneous tissue (the fatty layer below the dermis). The exact cause is often unknown, but genetics can play a role, and they sometimes appear after blunt trauma to an area.
- Clinical Presentation: Typically present as soft, mobile, rubbery, painless lumps located just beneath the skin surface in the subcutaneous tissue. The overlying skin is usually normal. Common locations include the trunk, neck, back, arms, and thighs. They can vary greatly in size, from less than 1 cm to over 10-20 cm (giant lipomas). They are often multiple.
- Diagnosis: Usually diagnosed clinically based on their characteristic soft, mobile, painless feel and location in the subcutaneous tissue. If the diagnosis is uncertain (e.g., hard, fixed, rapidly growing, painful lump), imaging (ultrasound, MRI) may be used to confirm the fatty nature and depth, or a biopsy may be needed to rule out rarer malignant fatty tumors (liposarcomas).
- Management: Lipomas are benign and do not need to be removed for medical reasons if the diagnosis is certain and they are asymptomatic. Removal is typically performed via surgical excision if they are painful (e.g., pressing on a nerve), growing rapidly, located in an area causing functional issues, large, or if the patient desires removal for cosmetic reasons. Excision is curative.
Sebaceous Hyperplasia
- What it is: This is a common benign condition characterized by enlarged oil glands (sebaceous glands). While often felt as a small bump, it is not a true cyst or nodule in the same way as an epidermoid cyst or lipoma, as it doesn’t have a sac-like structure or form a large, deep mass. Patients sometimes perceive them as stubborn whiteheads that won’t go away.
- Clinical Presentation: Presents as small, yellowish or flesh-colored bumps, typically 1-5 mm in diameter, often with a central indentation or pore. Common locations are the face (forehead, cheeks, nose). They are more common with age, sun damage, and in individuals with oily skin.
- Diagnosis: Usually diagnosed clinically by a dermatologist based on their characteristic appearance. Biopsy is rarely needed unless the diagnosis is uncertain (e.g., needing to rule out a basal cell carcinoma, which can sometimes look similar).
- Management: Sebaceous hyperplasia is harmless. Treatment is usually for cosmetic reasons. Options include gentle extraction (contents are oily, not cheesy keratin), shave excision, electrocautery (using heat), or laser treatment (e.g., CO2 laser). Recurrence is common as the underlying tendency for glands to enlarge remains.
Dermatofibromas
- What it is: These are common benign fibrous growths in the dermis. They are often felt as firm bumps.
- Formation: The exact cause is unknown, but they often seem to appear after minor trauma, an insect bite, or a follicle rupture. They are composed of an overgrowth of fibroblasts and collagen.
- Clinical Presentation: Present as firm, reddish-brown to dark brown bumps, typically 0.5 to 1 cm in diameter. Common locations are the legs and arms, but they can occur anywhere. They may feel like a hard “button” or small pebble under the skin. A characteristic sign is the “dimple sign,” where the lesion dimples inwards when squeezed from the sides. They are usually asymptomatic but can sometimes be itchy, tender, or slightly painful.
- Diagnosis: Usually diagnosed clinically based on their appearance, feel, and the dimple sign. Biopsy may be performed if the diagnosis is uncertain (e.g., needing to rule out a melanoma or other growth), if the lesion is growing rapidly, or if it is symptomatic.
- Management: Dermatofibromas are benign and do not need to be removed unless they are symptomatic (itchy, painful, growing), cosmetically bothersome, or if the diagnosis is uncertain and biopsy is required. Removal is done via surgical excision, which results in a scar (often larger than the lesion itself due to the need to remove enough tissue for closure).
These are just some of the most common types of benign nodules and cysts a dermatologist encounters. Many other less common benign growths can also present as skin lumps.
Common Inflammatory Nodules and Cysts: Lumps Caused by Inflammation
Some types of skin nodules and “cysts” are primarily driven by inflammation, often related to infections or specific inflammatory conditions.
Acne Nodules and Cysts (Severe Acne Vulgaris)
- What they are: These are the most severe forms of inflammatory acne lesions, occurring deep within the skin. While often called “acne cysts,” they are not true cysts with an epithelial lining in the same way as epidermoid cysts. They are large, deep, painful inflammatory nodules.
- Formation: They form when the contents of a blocked and inflamed hair follicle (oil, bacteria, keratin) rupture deep into the surrounding dermis and subcutaneous tissue. This triggers a strong, intense inflammatory response.
- Clinical Presentation: Present as large, painful, red, swollen lumps under the skin. They can persist for weeks or even months. They are most common on the face, chest, and back. They are associated with significant inflammation and have a high risk of causing permanent acne scars (atrophic or hypertrophic).
- Diagnosis: Diagnosed clinically as part of the overall presentation of severe acne vulgaris, along with other acne lesions like papules, pustules, and comedones.
- Management: Treatment for acne nodules and cysts is primarily focused on controlling the underlying severe inflammatory acne.
- Medical Management: Oral medications are usually necessary. Oral antibiotics (e.g., tetracyclines) are used for their anti-inflammatory effects and to reduce bacteria. Oral retinoids like isotretinoin are the most effective treatment for severe, nodular, and cystic acne, targeting all four main factors involved in acne formation (oil production, clogging, bacteria, inflammation) and often leading to long-term remission. Hormonal therapies can also be used in women.
- Intralesional Corticosteroid Injection: A dilute corticosteroid solution can be injected directly into individual large, painful acne nodules or cysts. This helps to rapidly reduce inflammation, swelling, and pain, and can minimize the risk of scarring from that specific lesion. Simple Explanation: A doctor injecting a small amount of anti-inflammatory medicine directly into a big, sore pimple to make it go down faster.
- Drainage: Simple incision and drainage of acne nodules/cysts is often not recommended unless there is a clearly visible collection of pus that has come to a head (forming an abscess). Draining deep, solid inflammatory nodules can be ineffective and may worsen scarring.
Hidradenitis Suppurativa (HS)
- What it is: A chronic inflammatory skin condition affecting hair follicles, primarily in areas with many apocrine sweat glands and hair follicles, such as the armpits (axillae), groin, perianal area, under the breasts, and buttocks. It is characterized by recurrent, painful nodules, abscesses, sinus tracts (tunnels under the skin), and scarring. It is not an infection caused by poor hygiene.
- Clinical Presentation: Typically begins with deep, painful nodules in the characteristic locations. These often develop into abscesses (collections of pus) that may rupture and drain pus. The inflammation is recurrent in the same areas, leading to the formation of interconnected tunnels under the skin (sinus tracts) and significant scarring. HS occurs after puberty and can range in severity from mild (a few recurrent nodules) to severe (extensive tunnels, draining pus, severe scarring).
- Diagnosis: Diagnosed clinically based on the characteristic lesions (recurrent nodules, abscesses, sinus tracts, scarring) in the typical locations. There is no specific diagnostic test for HS itself, although cultures of pus may be taken to identify secondary bacterial infections, and biopsies may be done if the diagnosis is uncertain initially.
- Management: Management of HS is complex and depends on severity. It often involves a combination of medical therapies and procedures.
- Medical Management: Antibiotics (oral and topical) are used to target bacteria (secondary infection) and for their anti-inflammatory effects. Intralesional corticosteroids are used for individual painful nodules. Hormonal therapies may be helpful for some women. Oral retinoids are sometimes used, but their effectiveness is variable. Newer treatments include biologic medications that target specific inflammatory pathways (e.g., adalimumab), which have proven effective for moderate to severe HS. Simple Explanation: Strong injectable medications that calm down the overactive inflammation causing the problem.
- Procedural/Surgical Management: Incision and Drainage (I&D) is used to manage painful, fluctuant abscesses, providing temporary relief but not addressing the underlying disease. Wide surgical excision of affected areas containing recurrent nodules, abscesses, and sinus tracts is often necessary for chronic or severe disease to remove the source of recurring inflammation, although it results in scarring. Laser treatments (e.g., CO2 laser) can also be used to destroy sinus tracts or affected tissue.
Abscesses
- What they are: Abscesses are localized collections of pus that form due to bacterial infection in the skin or subcutaneous tissue. They are often caused by bacteria entering through a break in the skin (e.g., a cut, insect bite, or a ruptured cyst or follicle).
- Clinical Presentation: Present as a painful, tender, warm, red, swollen lump. As the infection progresses, the center may become softer and feel like it contains liquid (fluctuant) as pus accumulates, and it may eventually come to a head and rupture, draining pus. Fevers and chills can occur, especially with larger abscesses.
- Diagnosis: Usually diagnosed clinically based on the characteristic signs of localized infection (pain, redness, swelling, warmth, fluctuation). Cultures of the pus may be taken to identify the specific bacteria causing the infection.
- Management:
- Incision and Drainage (I&D): The primary and most effective treatment for a mature abscess that is fluctuant. A cut is made in the skin over the abscess, and the pus is drained out. The cavity is often packed with gauze to allow continued drainage. Simple Explanation: Making a cut to let the pus out.
- Antibiotics: Antibiotics (oral or sometimes intravenous for severe infections) are often prescribed, especially if there is significant surrounding cellulitis (spreading skin infection), if the patient has signs of systemic illness (fever), or if they have underlying conditions that impair their immune system. Antibiotics alone are usually not sufficient to treat an abscess; drainage is usually necessary.
When Could a Nodule or Lump Be Malignant (Skin Cancer)?
It is a crucial point in dermatology that any new or changing lump or bump on the skin must be evaluated by a medical professional to rule out malignancy (skin cancer). While most skin cancers appear as patches or non-healing sores, some types can initially present as nodules or lumps.
Types of skin cancers that can present as nodules include:
- Basal Cell Carcinoma (BCC): The most common type of skin cancer. While often presenting as a pearly bump with visible blood vessels, it can grow into a larger nodule over time. It is typically slow-growing.
- Squamous Cell Carcinoma (SCC): The second most common type of skin cancer. Can appear as a firm, red, often tender nodule with a rough, scaly, or crusted surface. It may bleed easily and not heal.
- Melanoma: The most dangerous type of skin cancer. While many melanomas are flat or asymmetrical spots with irregular borders and changing colors, some melanomas can grow into a raised nodule that is dark, black, or even flesh-colored or red. Nodular melanoma can grow rapidly.
- Merkel Cell Carcinoma: A rare but aggressive type of skin cancer that typically appears as a firm, painless, shiny, flesh-colored to reddish-purple nodule that grows rapidly.
- Cutaneous Metastases: Cancers from internal organs or other parts of the body can sometimes spread to the skin, appearing as single or multiple hard nodules.
Warning Signs for any Skin Lump or Bump:
Be vigilant and seek prompt medical evaluation if you notice any skin lump or bump that:
- Is new and growing rapidly.
- Is changing in size, shape, or color.
- Bleeds easily or spontaneously.
- Does not heal within a few weeks.
- Is firm, hard, or fixed (not easily movable).
- Is unusually painful or tender without clear signs of infection.
- Appears significantly different from your other moles or skin lesions (“ugly duckling sign”).
The only definitive way to confirm if a nodule or lump is benign or malignant is through a biopsy followed by histopathological examination by a dermatopathologist. This is why dermatologists often recommend removing or taking a sample of suspicious or uncertain lesions for testing.

Treatment Modalities for Nodules and Cysts
The treatment for skin nodules and cysts varies greatly depending on the specific diagnosis, size, location, symptoms, and whether the lesion is benign, inflammatory, or malignant.
- Observation: For asymptomatic lesions that are clearly diagnosed as benign based on clinical examination (e.g., a classic lipoma or epidermoid cyst without inflammation) and where the diagnosis is certain, observation may be the recommended approach. The patient is advised to monitor the lesion for any changes and return if it grows, becomes painful, or changes in any concerning way.
- Incision and Drainage (I&D): This is the primary treatment for infected or inflamed cysts or abscesses that are fluctuant (contain pus). It provides immediate relief of pain and swelling by allowing the pus to drain. However, for cysts, it does not remove the sac lining, so the cyst is likely to recur once the inflammation subsides. For abscesses, it is usually combined with antibiotics.
- Intralesional Injection: Injection of medication (most commonly a diluted corticosteroid) directly into the lesion. This is particularly effective for reducing inflammation, pain, and swelling in inflammatory nodules, such as acne cysts or inflamed epidermoid cysts. It can help speed healing and reduce scarring. It does not remove the lesion itself, although inflamed cysts may resolve after injection.
- Medical Management: For inflammatory conditions that cause nodules or cysts (e.g., severe acne vulgaris, hidradenitis suppurativa), medical therapy targeting the underlying inflammation and infection is often the primary approach. This may involve oral antibiotics, oral retinoids (like isotretinoin for acne), hormonal therapies, or newer biologic medications (for severe HS). Procedures like I&D or surgery may be used adjunctively.
- Surgical Excision: This is the most common method for the complete removal of benign skin tumors (like lipomas) and cysts (epidermoid cysts, pilar cysts), and for removing lesions where malignancy is suspected or confirmed.
- Procedure: Performed in a clinic or hospital setting under local anesthetic (numbing the area). An incision is made in the skin over the lesion. The practitioner carefully dissects the lesion (e.g., removes the entire cyst sac intact, or removes the fatty tumor) from the surrounding tissue. The incision is then closed with sutures (stitches). The removed tissue is usually sent for histopathological examination to confirm the diagnosis.
- Goal: For cysts, the goal is to remove the entire sac lining to prevent the cyst from growing back (recurrence). For lipomas, it’s to remove the fatty mass. For suspected malignancy, it’s to remove the lesion with adequate margins.
- Outcome: Surgical excision results in a permanent scar. The size and appearance of the scar depend on the size and location of the removed lesion, the surgical technique used, and the individual’s tendency for scarring.
- Minimally Invasive Excision Techniques for Cysts: For epidermoid cysts, techniques aimed at minimizing scarring can be used. One approach involves making a very small incision (e.g., 2-3 mm) over the punctum, expressing the cyst contents, and then carefully removing the cyst sac lining through the small opening. While aiming for a smaller scar, there might be a slightly higher risk of recurrence compared to traditional wide excision if any part of the sac lining is left behind.
- Other Ablative Techniques: For certain small, benign bumps like sebaceous hyperplasia or small dermatofibromas, techniques that destroy or remove the lesion on the surface can be used instead of formal excision with closure. This includes shave excision (shaving the lesion off the surface), electrocautery (using heat to destroy the tissue), or laser ablation (using a CO2 laser to vaporize the tissue). These techniques typically result in a wound that heals on its own (secondary intention) and can leave a small scar or pigment change.
- Management of Malignant Lesions: If a biopsy confirms malignancy, the treatment approach depends on the type and stage of the skin cancer. This usually involves wider surgical excision with specific margins defined by treatment guidelines, or sometimes other therapies like radiation or topical chemotherapy.
The specific treatment chosen for a nodule or cyst is always based on the accurate diagnosis established by a medical professional.
Potential Complications of Nodules and Cysts (and their Treatment)
While most nodules and cysts are benign, they can be associated with complications, and the treatments used to manage them also carry potential risks.
- Inflammation and Infection: Benign cysts, particularly epidermoid cysts, are prone to becoming inflamed or infected. This causes pain, redness, swelling, and can lead to abscess formation. Inflammatory nodules (like acne cysts, HS lesions) are inherently inflamed and can become secondarily infected.
- Rupture: Cysts can rupture under the skin, leading to an intense inflammatory reaction to the keratin contents.
- Pain and Discomfort: Lumps can be painful if they become inflamed or infected, if they are located in an area subject to pressure or friction, or if they press on underlying nerves. Inflammatory nodules (acne, HS) are often significantly painful.
- Scarring: Scarring is an inevitable outcome of healing whenever the dermis is injured, whether from inflammation, rupture of a lesion, or surgical removal. The appearance of the scar depends on the size and depth of the original lesion or surgical wound, its location on the body, the surgical technique, and individual factors (e.g., tendency towards hypertrophic scars or keloids). Scarring is a significant concern with severe inflammatory acne and HS.
- Recurrence: Cysts can recur if the entire cyst sac lining is not completely removed during excision or if they are only incised and drained when inflamed. Lipomas can recur in the same area if not fully removed, or new lipomas can develop elsewhere (as they are often multiple). Inflammatory conditions like acne and HS are chronic, and while treatments manage flares, the underlying disease persists.
- Bleeding and Bruising: Can occur during or after biopsy or surgical excision.
- Hematoma/Seroma: A collection of blood (hematoma) or fluid (seroma) can accumulate under the skin after surgery, sometimes requiring drainage.
- Infection: Infection at the site of a biopsy or surgical incision is a potential risk, although uncommon with proper sterile technique and wound care.
- Nerve Damage: A rare risk with surgery, depending on the location of the lesion and proximity to nerves, which can result in temporary or permanent numbness or weakness.
- Pigment Changes: Redness or post-inflammatory hyperpigmentation (darkening) can occur at the site of previous inflammation or after surgical healing, especially in individuals with darker skin types. Hypopigmentation (lightening) is also possible with scarring.
An experienced practitioner will discuss the potential risks and complications of your specific lesion and the recommended treatment plan, and will take steps to minimize these risks.
The Consultation Process in Antalya for Nodules and Cysts
Seeking Nodules and Cysts Treatment in Antalya begins with a consultation with a qualified dermatologist or, for deeper or more complex lesions, potentially a general surgeon or plastic surgeon specializing in skin and soft tissue procedures. The consultation is crucial for proper diagnosis and treatment planning.
During the consultation, the medical professional will:
- Take a Detailed History: Ask about your symptoms, when the lump appeared, how it has changed, any associated pain or discharge, history of similar lesions, and relevant medical history.
- Perform a Thorough Clinical Examination: Carefully examine the nodule or cyst, assessing its size, shape, consistency, mobility, tenderness, color, surface characteristics, and location. They will also check for other skin lesions.
- Discuss Potential Diagnoses: Based on the clinical findings, they will discuss the most likely diagnoses for your lesion(s), explaining what each means in simple terms. They will discuss whether the appearance is classic for a specific benign lesion or if there are any features that raise suspicion for malignancy.
- Recommend Diagnostic Procedures (If Needed): If the diagnosis is uncertain, or if there are any concerning features, they will explain why a biopsy is recommended, what type of biopsy is appropriate, how it is performed, and what information they expect to gain from the histopathology results.
- Discuss Treatment Options: Based on the likely or confirmed diagnosis, they will discuss the recommended treatment options. This might include observation, medical management (for inflammatory conditions), incision and drainage (for infected lesions), or surgical removal (excision). They will explain the rationale for the recommended treatment.
- Explain the Procedure (If Recommended): If a procedure (like biopsy or excision) is recommended, they will explain how it is performed, the type of anesthetic used (usually local), what sensations you can expect during the procedure, the expected duration, and where it will be performed (clinic or minor surgery room).
- Discuss Potential Risks and Complications: Explain the potential risks and complications associated with the specific lesion (e.g., inflammation, infection, recurrence) and the recommended treatment (e.g., scarring, infection, bleeding, recurrence after I&D vs. excision).
- Discuss Expected Outcome and Recovery: Explain what outcome to expect from the treatment (e.g., complete removal with excision, control of inflammation with medical therapy, scar formation). Detail the expected recovery time, wound care instructions, and when you can return to normal activities.
- Provide Cost Information: Clearly outline the estimated cost of the consultation, any diagnostic procedures (like biopsy and histopathology), and the recommended treatment (e.g., cost of excision).
- Answer All Your Questions: Provide ample time for you to ask any questions you have about your lesion, the potential diagnoses, the recommended investigations or treatments, or anything else.
Seeking a consultation with a qualified medical professional in Antalya ensures that your lump or bump is properly evaluated and managed based on medical expertise.
The Procedure Experience in Antalya
Undergoing a biopsy or surgical excision for a nodule or cyst in Antalya in a reputable clinic or hospital is typically a straightforward outpatient procedure performed under local anesthetic.
- Before the Procedure: The area around the lesion will be cleaned with an antiseptic solution. The practitioner will inject a local anesthetic (like lidocaine) into the skin around the lesion to numb the area. You may feel a brief stinging sensation from the injection, but the area will become numb shortly after.
- During the Procedure: Once the area is numb, you should not feel pain. You may feel pressure, pushing, or pulling sensations as the practitioner performs the biopsy or carefully dissects the lesion. You will be awake throughout the procedure. The practitioner will use sterile instruments. The size and depth of the incision will depend on the size and type of lesion being removed. For excisions, the incision will be closed with sutures (stitches), which may be dissolvable (absorbable) or non-dissolvable (requiring removal later).
- Immediately After the Procedure: The wound will be cleaned and a sterile dressing applied. You will be given instructions on how to care for the wound at home. You may experience some mild discomfort, bruising, or swelling in the area once the local anesthetic wears off, which can usually be managed with over-the-counter pain medication.
Reputable clinics and hospitals in Antalya adhere to high standards of hygiene and safety protocols for minor surgical procedures.
Recovery and Post-Treatment Care
Proper post-treatment care is essential for optimal healing, minimizing complications, and influencing the final appearance of any resulting scar after the treatment of nodules or cysts. The specific care depends on the type of procedure performed.
- For Biopsy Sites:
- Keep the area clean and dry as instructed (often for the first 24 hours).
- Change the dressing as directed by your practitioner.
- Avoid picking at the site.
- Keep the site protected from excessive sun exposure to minimize pigment changes.
- Expected healing time is typically 1-2 weeks for most biopsy sites.
- For Surgical Excision Sites:
- Keep the wound clean and dry as instructed (often for the first 24-48 hours).
- Change the dressing regularly as directed.
- If non-dissolvable sutures were used, you will need to return to the clinic to have them removed, typically within 7-14 days depending on the location.
- Avoid strenuous activity that puts tension on the incision line, as this can widen the scar.
- Recognize and report any signs of infection (increased redness, swelling, pain, warmth, pus) to your practitioner.
- Once the wound is healed and sutures are removed, begin scar management as recommended by your practitioner (e.g., gentle massage, silicone sheets or gel, avoiding excessive sun exposure). Sun protection of the healing scar is crucial for minimizing hyperpigmentation.
- Expected healing time for the incision to close is typically 1-2 weeks, but the scar will continue to mature and improve in appearance over several months to a year or more.
- After Incision and Drainage (I&D) of an Abscess:
- Follow instructions for cleaning and dressing the drainage site. The site may need to be packed with gauze initially.
- Complete any prescribed course of antibiotics.
- Keep the area clean to prevent further infection. The wound will heal from the bottom up.
- After Intralesional Injections: Minimal specific care needed for the injection site, beyond general cleanliness. Monitor the lesion’s response to the injection over the following weeks.
Follow all specific post-treatment instructions provided by your medical professional in Antalya for the best possible healing and outcome.
Results and Expectations from Treatment
The results and expected outcomes from the treatment of nodules and cysts depend entirely on the initial diagnosis and the specific treatment approach used.
- Benign Lesions (e.g., Epidermoid Cyst, Pilar Cyst, Lipoma):
- Excision: If the entire lesion (including the cyst sac for cysts) is completely removed, the result is typically curative. The lesion will not grow back in that exact spot (although new ones can form elsewhere). The outcome is the removal of the lump, but this is replaced by a scar. The goal is for the resulting scar to be as minimal and aesthetically pleasing as possible.
- I&D (for inflamed/infected cysts): Provides relief of inflammation and pain, but does not remove the cyst sac, so recurrence of the cyst is likely once the inflammation resolves.
- Observation: The lump remains unchanged unless it becomes symptomatic or changes in appearance.
- Inflammatory Conditions (e.g., Acne Nodules/Cysts, HS, Abscesses):
- Medical Management: Aims to control inflammation, reduce flare frequency and severity, and minimize scarring. Results are seen over weeks to months with consistent medication use. The underlying conditions (acne, HS) are often chronic and require ongoing management.
- Intralesional Injection: Can cause rapid reduction in the size and inflammation of an individual lesion. Does not treat the underlying condition.
- I&D (for abscesses/HS abscesses): Provides relief from infection/pus collection but does not address the underlying cause or prevent future lesions.
- Surgical Excision (for HS): Aims to remove affected areas to reduce recurrent inflammation and tunneling but results in significant scarring.
- Malignant Lesions: If a biopsy confirms malignancy, the goal of treatment is complete removal of the cancer with adequate margins to prevent recurrence and spread. Prognosis depends on the type and stage of the cancer.
Histopathology Results: If a biopsy or excision was performed, the histopathology report from the pathologist is crucial. It provides the definitive diagnosis and guides further management. Your practitioner will discuss these results with you once they are available.
Scarring: It is important to have realistic expectations about scarring. Removal of a nodule or cyst that requires an incision will result in a scar. Scar appearance improves significantly over the first year or two as it matures, but it is permanent. Factors influencing scar appearance include genetics, location, size of the excision, closure technique, wound healing, and sun exposure during healing.
Nodules and Cysts Treatment in Antalya: Why Choose Turkey?
Turkey has become a prominent destination for medical tourism, and seeking Nodules and Cysts Treatment in Antalya offers access to a range of medical expertise and facilities. Several factors contribute to its appeal for individuals seeking evaluation and treatment for skin lumps:
- Qualified Medical Professionals: Antalya has a significant number of highly trained and experienced dermatologists, as well as general surgeons and plastic surgeons specializing in skin and soft tissue procedures. You can find practitioners skilled in diagnosing various types of nodules and cysts, performing biopsies, administering intralesional injections, and performing surgical excisions.
- Access to Diagnostic Services: Reputable clinics and hospitals in Antalya have access to necessary diagnostic services, including facilities for performing skin biopsies and sending tissue samples for histopathological examination by qualified dermatopathologists. This is crucial for accurate diagnosis, especially when malignancy is suspected or needs to be ruled out.
- Modern Facilities: Many clinics and hospitals in Antalya are modern, well-equipped, and maintain high standards of hygiene and patient care for minor surgical procedures performed under local anesthetic.
- Cost-Effectiveness: The cost of dermatological consultations, diagnostic procedures (like biopsy and histopathology), and minor surgical excisions in Turkey is generally lower compared to many countries in Western Europe, North America, and other regions. This makes receiving expert evaluation and treatment more accessible.
- Established Medical Tourism Infrastructure: Antalya has a well-developed infrastructure supporting medical tourists, including clinics that cater to international patients, often offering services in multiple languages and assistance with logistics.
- Access to Timely Evaluation: For concerning lesions that require prompt evaluation to rule out malignancy, accessing a consultation with a dermatologist in Antalya is often possible in a timely manner.
Considerations When Choosing a Medical Provider for Nodules and Cysts Treatment in Antalya:
- Practitioner’s Credentials and Experience: For evaluating skin lumps, consult a qualified dermatologist. If surgical removal is required, they may perform it themselves (if they have surgical training and facilities) or refer you to a general surgeon or plastic surgeon specializing in skin and soft tissue excisions. Verify their qualifications and experience in diagnosing and treating various types of skin lesions.
- Clinic/Hospital Reputation: Research the reputation of the clinic or hospital. Look for patient reviews, especially those related to dermatology or minor surgery.
- Access to Histopathology: Crucially, confirm that any removed tissue will be sent for histopathological examination by a qualified dermatopathologist, especially if the diagnosis is uncertain or malignancy is a possibility.
- Communication: Ensure clear communication with the medical staff and practitioner regarding diagnosis, treatment options, risks, recovery, and any histopathology results.
- Post-Treatment Support: Understand the instructions for post-treatment care and how follow-up will be handled, especially if you are traveling.
Choosing a qualified and experienced medical professional who prioritizes accurate diagnosis and uses appropriate procedures is essential for the effective and safe management of nodules and cysts in Antalya.
Conclusion
Skin nodules and cysts are common types of lumps or bumps that can develop on the skin and in the underlying subcutaneous tissue. While many are benign (non-cancerous), they can be bothersome due to their size, location, potential for inflammation or infection, or cosmetic appearance. Critically, some skin cancers or inflammatory conditions can also present as nodules or lumps. Therefore, it is paramount to seek professional evaluation by a dermatologist for any new, changing, or symptomatic skin lump.
A dermatologist’s approach to diagnosis involves a thorough clinical examination, detailed patient history, and often a skin biopsy with histopathological examination – the definitive method for determining the exact type of lesion and ruling out malignancy. Common benign types include epidermoid cysts (often miscalled “sebaceous cysts”), pilar cysts, and lipomas. Inflammatory causes include acne nodules and cysts, hidradenitis suppurativa, and abscesses. Recognizing the potential for malignant lesions (like BCC, SCC, melanoma) is a key reason why professional evaluation is necessary.
Treatment modalities vary based on the diagnosis, ranging from observation for asymptomatic benign lesions, medical management (antibiotics, retinoids, biologics) for inflammatory conditions, to surgical excision for complete removal of benign cysts and lipomas or for diagnostic purposes. Incision and Drainage (I&D) provides symptomatic relief for infected lesions but often does not prevent recurrence of cysts.
Considering Nodules and Cysts Treatment in Antalya offers access to qualified dermatologists and surgical facilities. Antalya has an established healthcare sector equipped to provide accurate diagnosis, necessary diagnostic procedures (including biopsy and histopathology), and various treatment options for skin lumps.
Understanding the importance of proper diagnosis, knowing the common types of nodules and cysts, and being aware of potential treatment options empowers individuals to seek timely and appropriate care. Consulting with a qualified dermatologist in Antalya for any concerning skin lump is the essential first step towards accurate diagnosis, effective management, and ensuring peace of mind regarding your skin health.
Discover the expertise of Dr. Ebru Okyay, your trusted dermatologist in Antalya. Whether you’re looking to address medical skin concerns or enhance your natural beauty with cosmetic treatments, Dr. Okyay is here to help. With personalized care and advanced techniques, achieving your skin goals has never been easier.